Table of Contents
Artificial urinary sphincter implantation
Artificial urinary sphincter (AUS) implantation is the standard treatment for moderate to severe stress urinary incontinence.
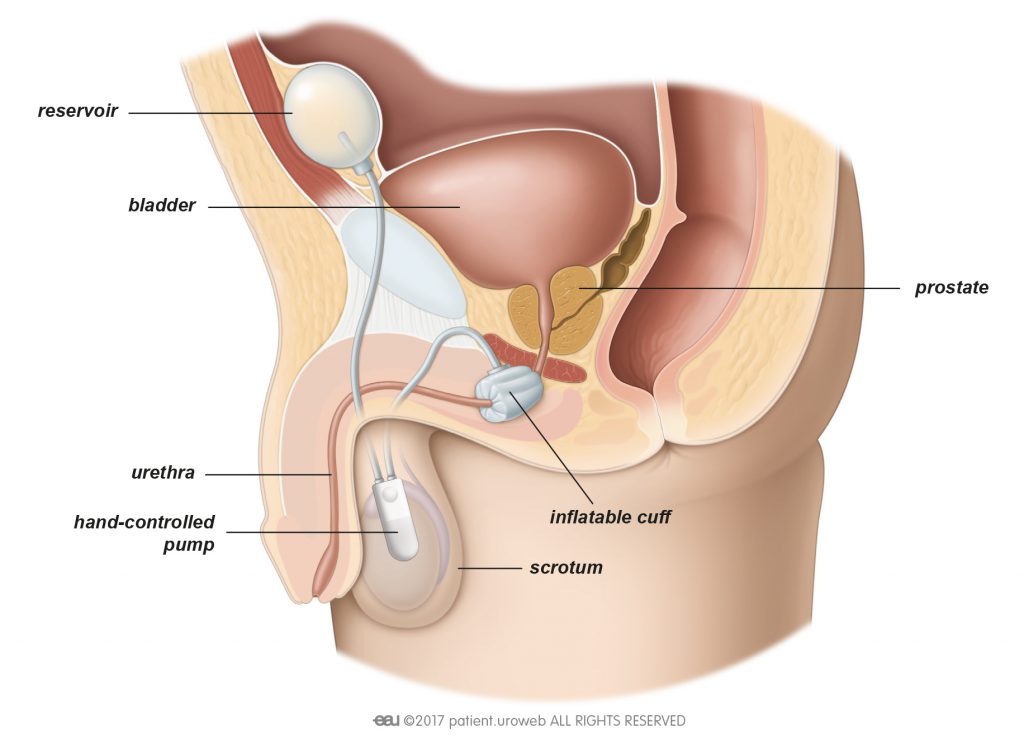
The AUS allows you to control your bladder with a hand-operated pump to compress and release a cuff around the urethra. The AUS consists of:
- An inflatable cuff placed around the urethra
- A reservoir to store liquid and keep the pressure in the system and placed into the belly
- A valve or pump to control the cuff and placed into the scrotum
The goal of the AUS is to reducte urine leakage during activities such as sneezing, coughing, running, or lifting weights.
The AUS can have complications, such as mechanical failure or infection, which implies its removal.
When is an AUS recommended?
AUS is generally recommended in case of severe urinary incontinence, or if sling implantation has failed to cure or improve your condition. AUS has a long-lasting effect and improves your quality of life.
You should be able to control the pump manually. Before the surgery is scheduled, the doctor or nurse will sit down with you to discuss how the device works and to make sure you feel comfortable using it.
The doctor will do some tests to make sure that there are no contraindications for getting an AUS. As part of this assessment, you may need a work-up including a urodynamic study, a cystoscopy, and a pad test.
How is the AUS implanted?
You will typically be asleep (general anaesthesia) for this procedure. Spinal anaesthesia can also be used to block nerve response to pain.
Steps:
- The bladder is emptied. The surgeon will insert a catheter to make sure that your bladder is completely empty during surgery.
- Incisions are made. An incision is made between the scrotum and the anus to place the cuff around the urethra, and another one in the lower abdomen to insert the reservoir.
- The AUS is placed. The cuff is placed around the urethra. Finally, the pump is positioned in the scrotum without any other incision and is connected to the other two elements of the device.
The cuff is left open until the doctor activates it a few weeks later in the outpatient clinic.
How to prepare for the procedure
Before surgery, the doctor will ask for a urine sample. This will be tested to make sure you do not have a urinary tract infection. If you have an infection this should be treated with antibiotics before scheduling the surgery. Your doctor may prescribe antibiotics before, during, and after the operation even if there is no infection, for the sake of preventing any infections.
Your doctor will advise you in detail about how to prepare for the procedure. If you need general anaesthesia you must not eat, drink, or smoke a certain time before surgery. If you are taking any prescribed medication, discuss it with your doctor. You may need to stop taking it several days before surgery. Your doctor will advise you on when you can start taking it again.
After the procedure
How long will it take me to get back to my daily activities?
This depends on the procedure performed. The doctor may remove the catheter right after the procedure or a couple of days after surgery. You can usually leave the hospital two or three days after implantation of an artificial urinary sphincter. You may need to stay in the hospital longer if you cannot urinate or your bladder does not empty itself completely, or if you have problems in the wound area such as an infection. The recommended length of hospital stay varies in different countries.
After you leave the hospital, your body still needs time to fully recover from surgery. Because of this, the AUS will not be activated until your lower urinary tract has completely healed. This means that in the weeks after the procedure you will continue to have urine leakage. During this time you may also experience pain in the pelvic area, or feel pain when you urinate. Your doctor can prescribe medication to deal with these symptoms.
The doctor will schedule an appointment to activate the device 4-6 weeks after surgery. Your wound will be checked as well. Usually, stitches that dissolve and disappear are used.
During the recovery period your doctor may recommend to:
- Consume enough liquid, especially water, to provide at least 2 litres of urine output
- Not lift anything heavier than 5 kilograms
- Not do any heavy exercise
- Take showers instead of baths
- Avoid thermal baths, or going to the sauna
- Prevent constipation by adapting your diet
- Avoid sexual activity
- Avoid activities which can traumatise the operation site, such as cycling and horseback riding.
Call your doctor or go back to the hospital right away if you:
- Have a fever
- Are unable to urinate on your own
- Have heavy blood loss or pain
- Notice the wounds start to bleed or leak transparent fluid, or hurts
- Notice swelling, pain, or redness in the scrotum