Table of Contents
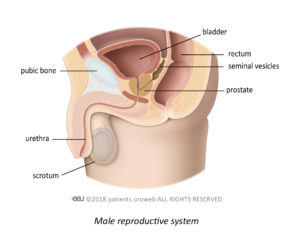
The prostate makes a thick white fluid which mixes with sperm from your testicles to make semen. It also produces a protein called prostate-specific antigen or PSA. PSA helps reduce the thickness of semen, so it becomes more liquid.
What is prostate-specific antigen (PSA)?
Prostate-specific antigen, or PSA, is produced by cells in the prostate. It is normal for small amounts of PSA to leak into your blood, and this amount increases as you get older because your prostate naturally gets bigger with age. PSA levels can be detected in your blood if you have a urine infection, but it could also be a sign of prostate cancer.
What is a PSA test?
A PSA test is a simple blood test that measures the level of PSA protein in your blood.
Who can have a PSA test?
If you are a man, trans woman, or a binary individual assigned male at birth, and over the age of 50, you can talk to your doctor about having a PSA test. You may be offered a PSA test as part of a general health check.
You can also talk to your doctor about having a PSA test if you are under 50 but have risk factors that are known to increase the chance of developing prostate cancer.
You do not have to have a PSA test; it is your choice. Some men choose not to have the test, while others want to rule out the possibility of prostate cancer. There is no right or wrong answer. You might find it helpful to discuss the possible advantages and disadvantages with your partner, family, friends, or prostate cancer support groups.
What else causes high levels of PSA in the blood?
Benign prostate enlargement
It is normal for the prostate to grow as a man gets older, but if it gets too big, it can put pressure on the urethra, making it difficult to pass urine. When this happens, it is called benign prostate enlargement or BPE. BPE can raise your PSA level, but it is not cancer. In most cases, BPE is not a serious health concern and is a treatable condition.
Chronic prostate pain syndrome
Some men experience painful swelling of their prostate, but the cause may not be obvious. This is called chronic prostate pain syndrome, or CPPS. CPPS is not a cancerous condition, but if your PSA level rises your doctor will arrange for you to have further tests to check for cancer.
Prostatitis
Sometimes bacteria can get into your prostate, causing it to become infected and inflamed. This condition is called prostatitis and can cause raised PSA levels in your blood. Although prostatitis can be a chronic condition, it is not cancerous, and can improve over time with treatment.
Urine infection
Urinary tract infections can raise your PSA level. If you have recently had a urinary tract infection, you will need to wait 4-6 weeks for the infection to clear before you have a PSA test. Discuss this with your doctor so he/she can arrange the most appropriate appointment date for you.
Prostate stimulation
Activities that stimulate your prostate, such as vigorous exercise (especially cycling) or ejaculation can raise your PSA level. Speak to your doctor about how long you should avoid these activities before having your PSA test checked again, but it is generally recommended to avoid these activities for a minimum of 48 hours.
Activities that massage the prostate, such as a prostate check or receiving anal sex, can also temporarily raise your PSA level. You may need to avoid these activities for a week before having your PSA level tested.
Medication
Certain medicines can affect your PSA level. Make sure you have a list of all your current medications to hand. You can then discuss your medications with your doctor, and he/she can consider the impact these may have on the interpretation of your PSA test results.
What happens during a PSA test?
Blood test
Your doctor, or a trained individual, will take a sample of your blood from a vein in your arm. A tight band, called a tourniquet, may be wrapped around your upper arm to temporarily slow down the flow of blood. This causes the vein to swell and makes it easier for a blood sample to be taken. A needle will be inserted into the vein and the blood drawn into a syringe. The blood sample will be sent to a laboratory to be tested.
Prostate check
You may also be offered a prostate check. A prostate check, or digital rectal examination (DRE), is a quick and simple test to see if you might have a prostate problem. You can read more about a DRE here.
Should I have a PSA test?
Sometimes, it can be difficult to decide whether or not to have a PSA test. Prostate cancer usually, but not always, grows slowly over many years. You may have prostate cancer that never causes symptoms or becomes a problem during your lifetime. Unfortunately, some men have prostate cancer that spreads rapidly throughout their body and ultimately leads to their death.
Possible advantages
- If the test result is normal, you may feel reassured.
- It can help find prostate cancer before you have any symptoms.
- It may help to find a fast-growing cancer at an early stage so you would have more treatment options to help stop the cancer from spreading, causing problems, and reduce the risk of dying prematurely.
Possible disadvantages
- A PSA test is not 100% accurate:
– You may have a high PSA level but do not have cancer.
– You may have a normal PSA level but have prostate cancer. - If your PSA level is raised, you may need more tests, which can be stressful for both you and your family.
- You could be diagnosed with a slow-growing prostate cancer and either not be offered treatment or have treatment that you did not need.
Your doctor may use a statistical program to predict your risk of prostate cancer. The results will help your doctor plan and discuss your treatment options with you. These programs are designed to be used by healthcare professionals, but if you are concerned about your prostate cancer risk, there are risk calculators suitable for patient’s to use.
Can I have regular PSA tests?
Several tests taken over time are more useful that a one-off test. But the need for regular PSA tests will be determined by your doctor based on your risk of developing prostate cancer and the usefulness of your first PSA test results.
Summary
- PSA testing helps finding prostate cancer at an early stage when it is more likely to be cured
- Remember, not everyone with a high PSA level will have a cancer and not everyone who is found to have a cancer will need treatment
- Talk to your family doctor about the risks and benefits and whether this test is right for you
The content on this page was produced by the EAU Patient Information Working Group. It contains general information about prostate cancer detection and does not replace an individual consultation.
Decision aid tools exist to help you decide whether or not to start an early detection pathway. None of these tools replace a consultation with your doctor. Talk to your doctor about the pros and cons of prostate cancer early detection before you decide if you want to be tested.
If you have any specific questions about your individual medical situation you should consult your doctor or other professional healthcare provider.