Table of Contents
What is varicocele?
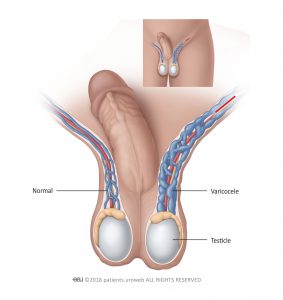
Varicocele describes a condition with swollen and enlarged veins in the scrotum (Figure 1). These veins carry blood from the testicles that is low in oxygen and nutrients. Swelling can happen when blood flows backward in the veins. Varicoceles are similar to varicose veins in the leg.
Varicoceles are common in prepubescent and adolescent boys. They are uncommon in boys younger than age 10 and rarely develop after adolescence. Most varicoceles are found only on the left side because of the way blood drains from the left testicle. In some cases they can also develop above the right or in both testicles.
Varicoceles usually are not painful and do not need treatment. However, treatment might be advised if a varicocele:
- Is painful
- Causes a testicle to underdevelop or shrink (testicular hypotrophy)
- Potentially affects the ability to father children (fertility)
In some cases, varicoceles can affect fertility by reducing blood flow and raising the temperature of the testicles. This can cause the testicles to produce fewer sperm, and sperm that is produced might not be healthy.
Cause of varicoceles
It is not known why varicoceles develop. They may be associated with accelerated sexual organ growth in young boys, but no specific risk factors have been determined.
The severity of a varicocele can be classified into three grades:
- Can be felt by hand only during straining
- Can be felt by hand when relaxed
- Can become clearly visible at a distance, even at complete rest
A varicocele may cause:
- Shrinkage of the affected testicle (atrophy). Most of the testicle is made up of sperm-producing tubules. When they are damaged, as from a varicocele, the testicle shrinks and softens. It is not clear what causes the testicle to shrink, but the malfunctioning valves allow blood to pool in the veins. This pooling can result in increased pressure in the veins that may cause testicular damage.
- Problems fathering children (infertility). With a varicocele, the testicle may be too warm. This can affect sperm formation, movement (motility), and function.
However, the majority of the boys with a varicocele will have no fertility problems later in life.
Symptoms and diagnosis of varicoceles
Varicoceles usually have no symptoms. In rare cases, it may cause pain, which may:
- Vary from sharp to dull discomfort in the scrotum
- Increase with standing or physical exertion
- Worsen over the course of the day
- Be relieved when you lie on your back
You may notice a varicocele, or it may be noticed by your parents or by a physician during a routine physical examination or during a fertility evaluation at an older age.
Varicoceles usually have no symptoms. In rare cases, it may cause pain, which may:
- Vary from sharp to dull discomfort in the scrotum
- Increase with standing or physical exertion
- Worsen over the course of the day
- Be relieved when you lie on your back
You may notice a varicocele, or it may be noticed by your parents or by a physician during a routine physical examination or during a fertility evaluation at an older age.
How is the diagnosis made?
It is usually relatively simple to diagnose a varicocele. Your doctor will take a detailed medical history and ask questions about your symptoms, if any.
Examination by a doctor is crucial to rule out or confirm a varicocele. Your doctor will carefully examine your external genitals. A collection of swollen and tangled veins in the scrotum that can be felt more in the upright posture or during straining, suggests a varicocele. The swollen veins may feel like a “bag of worms”. Both testicles should be examined to compare their size. The testicle affected by varicocele is usually smaller.
Backward flow of blood in the swollen testicular veins is usually confirmed by ultrasound of the scrotum.
A right-side-only varicocele is uncommon. In extremely rare cases, it might be caused by a tumour and ultrasound should be performed to rule it out.
Treatment of varicoceles
Surgery is the only way to treat varicoceles, but not all patients would benefit from surgery. Surgery may be recommended if:
- The affected testicle is small
- There exist other conditions associated that could affect fertility
- Varicocele is present in both testicles
- The sperm is not healthy (in older adolescents)
- Pain, marked swelling, or physical discomfort is present
If none of these criteria apply, surgery is not needed. Annual visits to the doctor are needed annually until sperm can be analysed.
Surgery
The surgical procedure blocks the enlarged veins from draining blood from the testicle (Figure 2). This blockage redirects the blood flow to healthy veins. This can be done:
- Through a small cut in the groin with the use of a surgical microscope
- Though multiple small cuts made with laparoscopic instruments
During surgery, the doctor will try to protect nearby structures called lymphatic vessels. These tiny structures are usually invisible to the naked eye. They carry lymph, a clear, yellowish liquid that collects in all parts of the body. If they are injured, lymph cannot flow properly, and complications can develop. This surgery, called lymphatic-sparing varicocelectomy , can lower the chance of complications.
What are the most common complications after surgery?
- Collection of fluid in the scrotum around the testicle (hydrocele formation)
- Shrinking of the testicle (testicular hypotrophy)
- Reduced function of the testicle
Angiographic occlusion
Less often, a procedure called angiographic occlusion is used to treat varicocele. It collapses the twisted vein with a special substance. This method does not usually require you to be asleep (general anaesthesia) and is less invasive than laparoscopic surgery. However, it uses X-ray, so you are exposed to radiation.
After surgery
The patient may be able to return to normal, nonstrenuous activities after 2 days. As long as they are not uncomfortable, they may return to more strenuous activity, such as exercising, after 2–4 weeks.
Pain from this surgery is usually mild but may continue for several days or weeks. The doctor may prescribe pain medication for a limited time after surgery. After that, the doctor may advise you to take over-the-counter medication like acetaminophen or ibuprofen. Wearing briefs or a jockstrap can also help by relieving pressure in the testicles.
It will take several months after surgery before improvements in sperm quality can be seen with a semen analysis. This is because it takes approximately 3 months for new sperm to develop.
Contact your doctor if you have questions or concerns.