Table of Contents
What is overactive bladder syndrome?
Overactive bladder syndrome, or OAB, is a common condition which can affect men, women, and children. Between 10% and 20% of people experience OAB at some stage in their lives and it most commonly affects women.
OAB alters how your bladder holds urine. If you have OAB, you may feel a sudden need or urge to urinate, even if your bladder isn’t very full. You also may find it difficult to hold urine in, so some urine may leak out.
People with OAB often need to urinate many times throughout the day but you may also find you wake up several times during the night needing to urinate too. This is known as nocturia. You can find out more about nocturia here.
OAB can be caused by an underlying medical condition. It is important to speak to your doctor if you have OAB symptoms, to find out if you have any other symptoms, such as blood in the urine, so as to investigate and, if necessary, treat the cause of your OAB symptoms.
Seeking help for overactive bladder syndrome
If you have OAB symptoms, it is important to seek medical advice. OAB symptoms can last for a long time. However, there are medicines and treatments that can help to ease and manage your OAB symptoms.
OAB symptoms can make it difficult to go about your everyday life and to do certain activities. They may make you feel self-conscious and affect your personal life and relationships.
Sometimes people feel embarrassed about their symptoms, they may think that OAB symptoms are just a part of ageing that should be accepted. This can put people off talking to their doctor about any urinary problems they are having.
Although it may feel difficult or uncomfortable to seek medical advice, it is important to speak to a doctor because it is very likely that something can be done to help you. OAB symptoms are not something to be embarrassed about, nor are they a normal consequence of getting older or having a baby.
The symptoms of OAB are bothersome rather than life-threatening, but it is important to seek medical advice in case they are caused by another medical condition, such as diabetes, or related to a problem in the nervous system, which would need to be diagnosed and treated.
What treatments are available for overactive bladder syndrome?
A specialist doctor will examine whether your symptoms are related to a certain cause (such as a bladder stone, or an infection) and then treat the underlying condition.
If an underlying medical condition is ruled out and your OAB symptoms remain, your doctor can look for the cause of your OAB symptoms and can discuss with you the options that are available to treat your symptoms. In many cases no underlying cause of OAB can be identified and focus is on treatment. This can help you to feel in control of your body, regain your quality of life and get back to work or other activities and hobbies that you might have stopped doing due to your symptoms.
There are a number of different treatments available for OAB. The treatment/s you are offered will vary depending on the type of symptoms you have, how severe they are, how they affect your life, your medical and surgical history, your personal preferences and beliefs, cultural aspects and the treatments available in your particular country.
Self-management of symptoms
As a first step, you may be advised by your doctor or other healthcare practitioner such as a nurse, to try some simple lifestyle changes that you can make yourself, such as:
- Adapting what, how much and when you are drinking liquids. Your healthcare provider can advise you how to do this.
- Drinking less in the evening so you are less likely to be woken up in the night with an urgent need to urinate.
- Reducing your intake of artificial sweeteners (which are often found in soft drinks), spicy foods, citrus fruits such as oranges, fruit juices, caffeine, and alcohol. These can irritate the bladder and worsen OAB symptoms.
- If you are having urine leakage, using an absorbent pad to protect your clothes.
- Trying to ‘hold’ your bladder (resisting the urge to urinate) for longer when you feel the need to go to the toilet. This can help to re-train your bladder so it can hold larger volumes of liquid, which will enable you to have longer time periods between toilet visits.
- Doing exercises to strengthen and relax your pelvic floor muscle. This can help you to regain muscle strength to help you overcome the urgent need to urinate. These exercises are given by a physiotherapist, so you know which exercises to do and how to do them correctly.
- Maintaining a healthy body weight. Being overweight increases the amount of pressure put on the bladder and can make it more likely that you will suffer from urine leakage if you have OAB.
These changes can help you to actively manage and potentially improve your OAB symptoms.
Medicines
If self-management does not help to control your OAB symptoms, your doctor may recommend a medicine or a combination of medicines. The goal is to reduce the urgent need to urinate, decrease the number of times you need to go to the toilet each day, and to prevent urinary leakage.
Medicines for OAB fall into two categories:
- Antimuscarinic medicines (there are several medicines in this category)
- Beta-3 agonist medicine (such as mirabegron)
Your doctor will discuss with you, the type of medicines that are available so you can decide together, which treatment is best for you.
The treatment options you are offered will be influenced by your age, symptoms and medical history, any other medications you are taking, the medicines available in your country and your personal preferences.
Many medicines cause mild to moderate side-effects and your doctor can discuss these with you, before you make any decisions about medical treatments. The advantage of medication is that if it doesn’t suit you, you can stop taking it and try something else. Furthermore, if either mirabegron or antimuscarinic alone is ineffective, both medications can be combined.
Antimuscarinics
Antimuscarinics, or muscarinic receptor antagonists are a group of medicines which help to treat OAB symptoms by reducing the messages sent to the brain telling you that “need to go to the toilet” as well as the number or strength of abnormal contractions (spasms) happening in the bladder. These medicines can also reduce urgency symptoms, so you don’t feel the need to urinate as urgently when you do need to go to the toilet.
Side effects of antimuscarinics
Antimuscarinic medicines can cause dry mouth, constipation, eyes feeling sensitive to light, hot and flushed skin, and fast heart rate. In rare cases, confusion, memory loss and worsening mental function (ability) can occur in older people. These symptoms should stop immediately when the medication is interrupted.
Antimuscarinic medicines are not suitable for women who are pregnant or breast feeding, people who have severe liver or kidney problems which stop these organs from working properly, people with a history of very high blood pressure, or people who are aged under 18 years.
There are several different antimuscarinic medicines so if one type causes side-effects that are problematic or make you feel unwell, your doctor may be able to offer you a different medicine. If taking the medicine in tablet form causes you to suffer with dry mouth, it may help to have your medicine via a skin patch (similar to a plaster) or ointment instead.
Beta-3 agonists
Beta-3 agonists are a type of drug that work by relaxing the bladder to reduce bladder contractions which would usually make you need to go to the toilet. This type of medicine improves OAB symptoms by increasing the amount of urine the bladder can hold so as to reduce the number of times you need to go to the toilet each day.
Beta-3 agonists are not suitable for people who are pregnant or breast feeding, people who have severe liver or kidney problems which stop these organs from working properly, people with a history of uncontrolled blood pressure, or people who are aged under 18 years.
Side effects of mirabegron
Mirabegron can sometimes cause an increase in your blood pressure, so it is important to have it checked after you have started taking it. Mirabegron may also cause urinary tract infection, diarrhoea, dizziness, headache, and difficulty urinating. If you experience any of these symptoms, it is important to contact your doctor right away.
If you are taking other medicines for different medical conditions, your doctor may consider changing these so that they don’t clash with any side-effects of medicines to treat your OAB.
It is important to note that just because a side effect is listed for a medicine, it does not mean that you will necessarily experience it. Some people do not notice any side effects at all when taking medicines for OAB.
Botulinum toxin
Botulinum toxin is a substance that is more commonly known to be used for cosmetic purposes. It is used to treat OAB symptoms by reducing the activity of the nerves in the bladder when self-management and medication have not been effective. Botulinum toxin relaxes the bladder reducing the urge to urinate as often or as urgently. It can also help to reduce urinary leaks for some people.
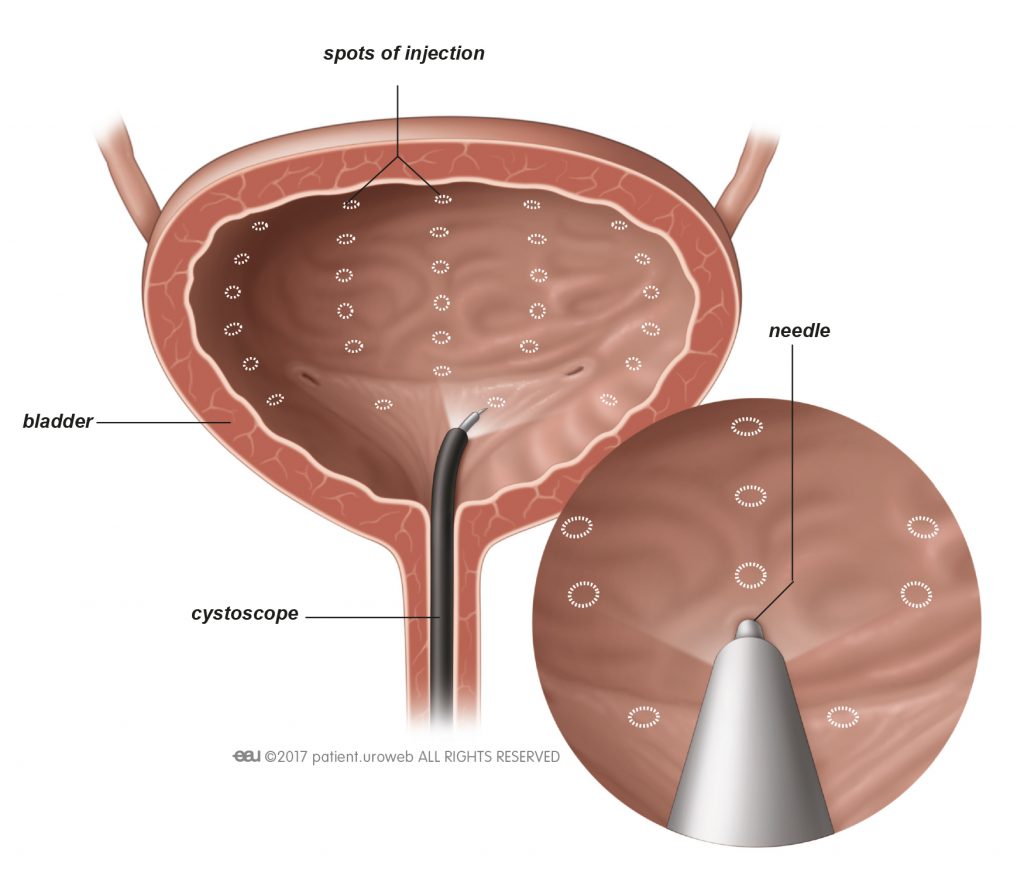
Botulinum toxin injections
Before the procedure, an anaesthetic fluid is inserted into the bladder to numb it. The doctor then uses a thin rod with a camera on the end, called a cystoscope, to inject the botulinum toxin into several places in your bladder wall. The cystoscope is inserted through your urethra and into your bladder. This procedure can also be done under general anaesthesia.
Botulinum toxin takes a week or two to take effect, but does wear off after a few months, so this is a treatment that needs to be repeated.
Side effects of botulinum toxin
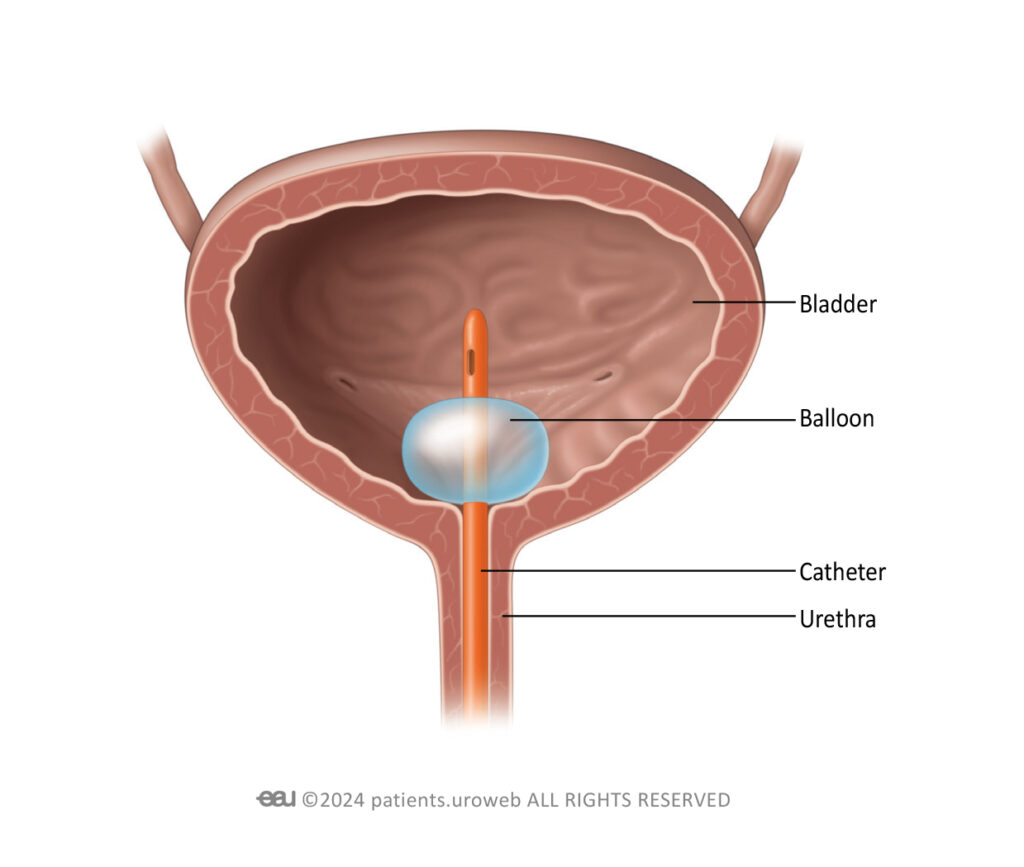
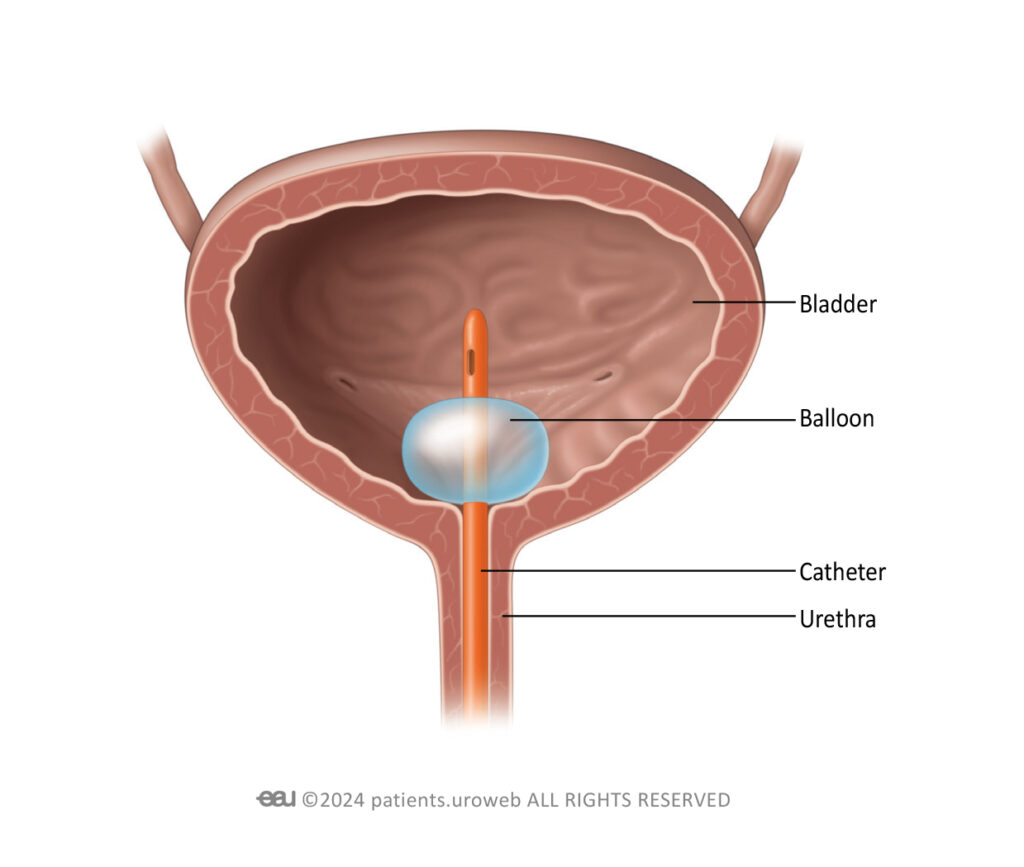
Less than 10% of people have difficulty emptying their bladder once they have had botulinum toxin injections into their bladder, depending on the dose of toxin used. This can be treated with a temporary catheter which is inserted as needed into the urethra to drain the bladder. If this is required, your medical team can teach you Clean Intermittent Self Catheterisation (CISC) whereby you are taught how to insert and remove a catheter at home yourself, so that you do not need to go to hospital or a medical clinic to have a catheter inserted. Alternatively, if you do not wish or are not able to do CISC, you can have an indwelling catheter temporarily inserted for a few days until your bladder recovers.
The procedure, as well as catheterisation if needed, can also cause urinary tract infections, which may require treatment with antibiotics.
Nerve stimulation
Nerve stimulation uses electrical pulses to regulate the nerves which control the bladder and brain responses. Your doctor may recommend nerve stimulation, or ‘neuromodulation’ as it is also known, if medicines haven’t been successful in treating your OAB symptoms or if you are unable to/would prefer not to take medication.
Nerve stimulation may not be suitable for you if you are pregnant or have a pacemaker fitted. You doctor can discuss this with you.
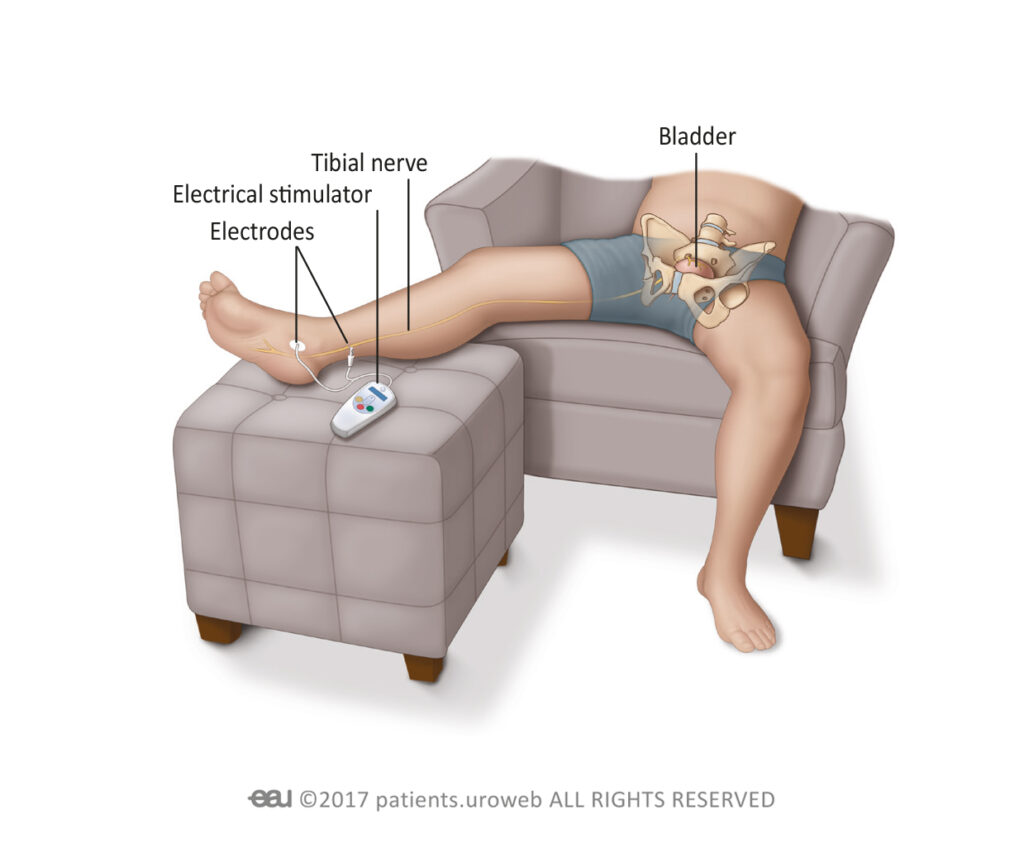
Tibial nerve stimulation
This procedure involves placing electrodes on the ankle to stimulate the tibial nerve, which runs from the inner part of the ankle, through the leg and to the nerves in the lower back. Tibial nerve stimulation is not painful, although you may feel a pulsing or tingling sensation in the foot during treatment.
You can perform tibial nerve stimulation at home. The treatment works by changing the pattern of messages sent via nerves to the bladder and pelvic floor. Your doctor will tell you how often you need to use the device (daily or weekly) and for what length of time (weeks or months).
Tibial nerve stimulation isn’t a permanent cure, so you may need further treatment courses over time.
Side effects of tibial nerve stimulation
No major side effects have been reported with tibial nerve stimulation.
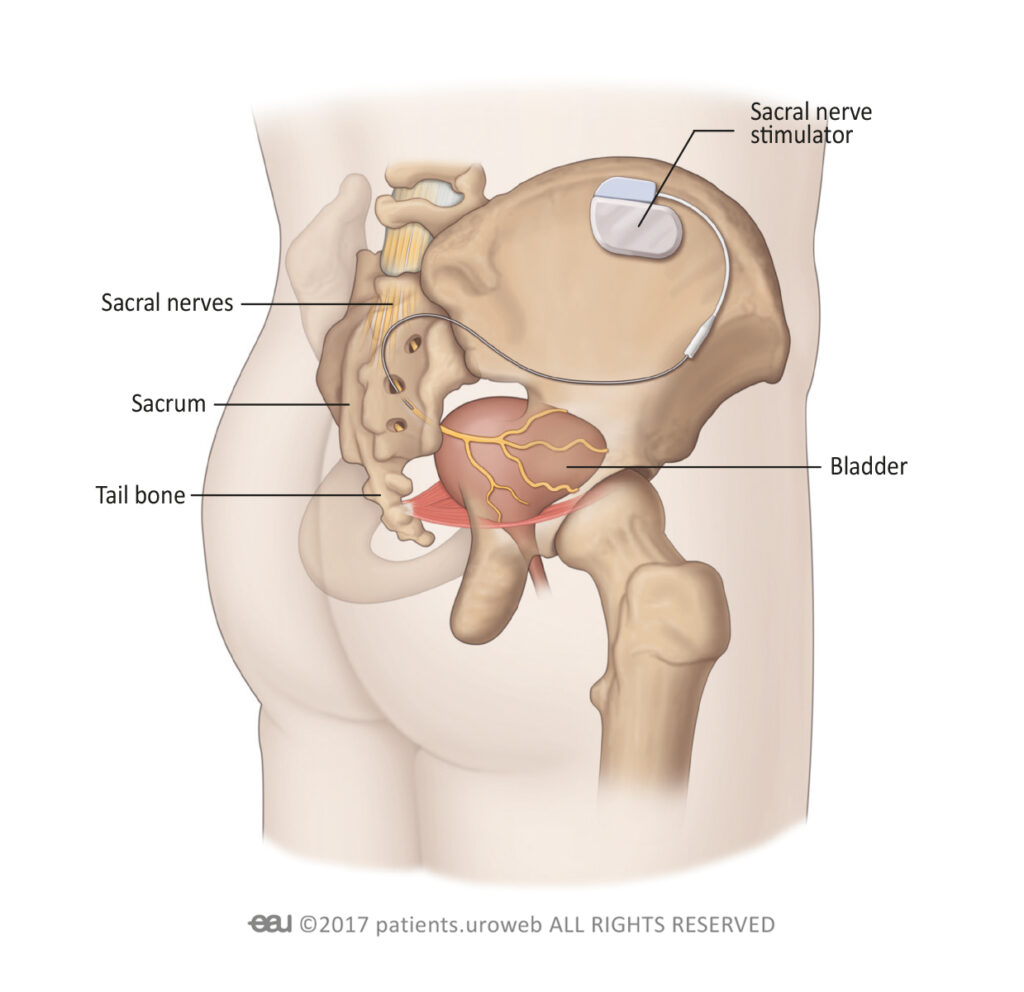
Sacral nerve modulation
Sacral nerve modulation is carried out in two stages. The first is a test stage, which is done to check if the treatment is likely to work for you. A doctor places an electrode through the skin into the lower back which remains in place for around a week. If you do not notice any improvement during this time, the electrode will be removed.
If the electrode does help to improve your symptoms, you will be offered surgery to implant a permanent device (which is similar to a pacemaker) just beneath the skin in the upper part of the buttock. There are different devices available (both portable and non-portable). Your doctor will discuss which devices are available to you and how each one works.
After surgery, you will be able to control the device yourself, through a hand-held controller. You can use this to remotely adjust the electrical stimulation that is sent to the nerves that control the bladder. This will normalise your bladder activity.
This type of treatment can greatly improve OAB symptoms as it provides treatment to the whole pelvic floor area.
Side effects of sacral nerve modulation
Following the procedure, there is a risk of infection, and you may experience pain in the area of the implant or electrode although this risk is very low. Over time, the implant or electrode may move, causing discomfort.
Surgery for OAB
If your OAB symptoms do not improve with self-management methods, medicines, or nerve stimulation treatments, you may be recommended to have surgery. The surgery can be done as open surgery or robot-assisted depending on the facilities available at your local hospital.
Bladder surgery
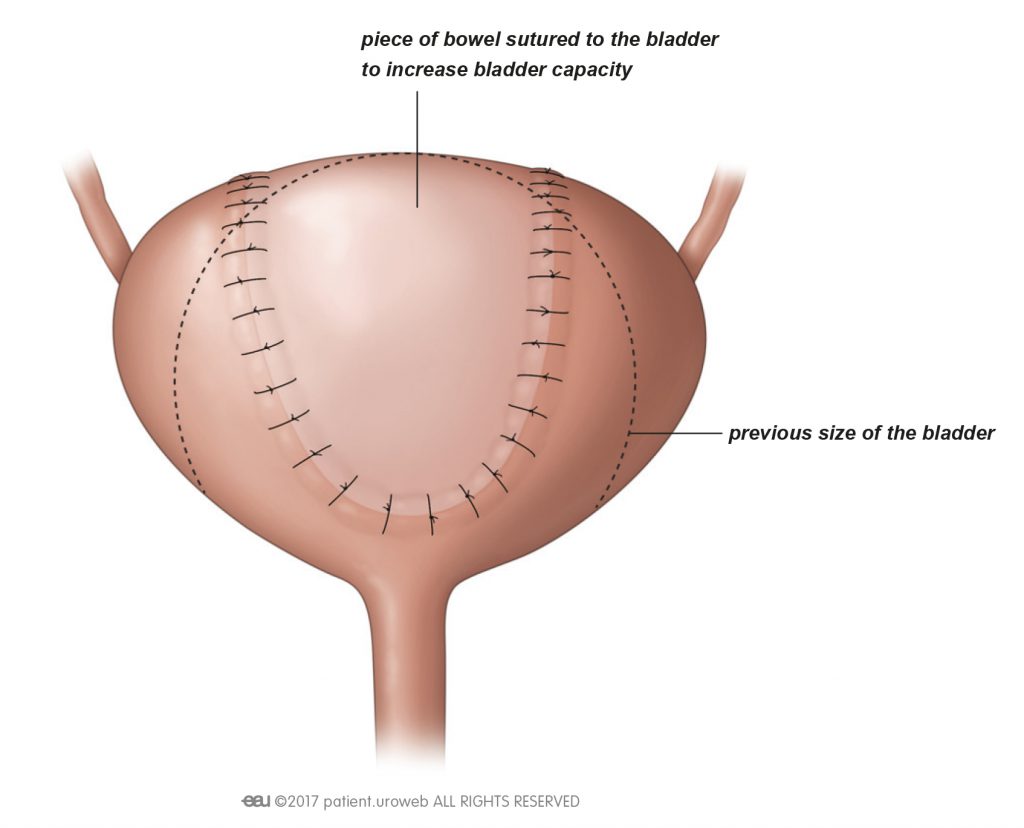
The main aim of the operation is to increase the size of your bladder so it can hold more liquid.
The surgery involves the doctor making a cut into your lower abdomen. A piece of your bowel is removed and is attached to your bladder to increase its size. During surgery, drainage tubes may be placed near your bladder to remove extra fluid. The medical name for this is bladder augmentation.
This type of procedure is not commonly carried out, as the surgery sometimes causes people to have difficulty urinating normally and a thin tube called a catheter may need to be inserted into your bladder through your urethra to help drain urine.
Things you may wish to consider when discussing surgery with your doctor:
- How your symptoms are affecting your quality of life.
- How well you are tolerating any medication you are currently taking.
- If your medical history makes you a suitable candidate for surgery.
- Your personal preferences.
Side effects of bladder surgery
After bladder surgery, if catheters are in place, there is a risk of mucus plugs forming in the catheter tubes. Mucus plugs can cause a blockage, which can prevent urine from draining properly and lead to discomfort and infection. It’s important to keep the catheter and drainage tubes properly drained to prevent mucus plugs from forming.
Around 1 in 10 patients may experience the following complications:
- Difficulty emptying the bladder
- Presence of mucus in the urine
- Recurring urinary infections
- Inadequate improvement of symptoms
- Symptoms returning at a later stage, that need further treatment
- Wound infection that may need antibiotics
Urinary diversion
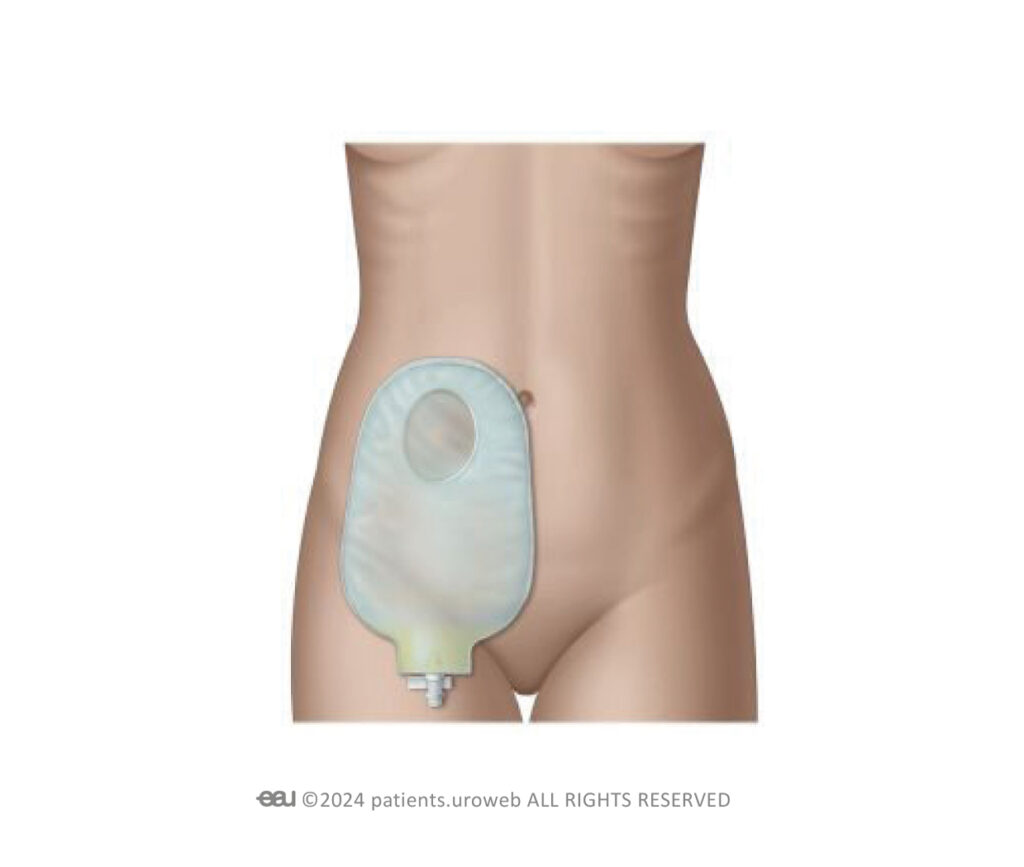
This procedure changes the path of the ureters, the tubes that carry urine from the kidneys to the bladder. The tubes are redirected through the abdominal wall and empty urine into a bag outside of your body. The bag is easy to take care for, and you will still be able to work and do physical activities.
Urinary diversion is normally only carried out if other treatments have not worked or are not possible.
Side effects of urinary diversion
The surgery can cause a few different problems, like a bladder infection, and sometimes people need more surgery to fix any issues that may occur.
Living with OAB
What is it like living with overactive bladder?
Overactive bladder syndrome can have a negative impact on your quality of life and lower your self-esteem. This can cause a strain on your relationships and sex life. It can be difficult to feel confident and attractive when you do not always feel in control of your body and if you are experiencing urinary leakage.
People with OAB may find they need to plan ahead to find toilet facilities. This may cause them to avoid trips to unknown places. The frequent need to urinate can also cause people to give up activities they used to enjoy, such as socialising or sports. It can also have an impact on work, such as suddenly needing to leave a meeting, or planning business trips.
Getting up at night to urinate can cause tiredness and affect your mood. You may also wake your partner by going to the toilet to urinate during the night.
It is important to talk to a doctor about your OAB symptoms if OAB is affecting your quality of life. You do not need to be embarrassed about your symptoms as doctors see and help many people with OAB.
Seeing a doctor is an important first step to taking back control. Your doctor will assess the effects of your OAB symptoms and can provide helpful advice on lifestyle changes and things you can do for yourself to improve your symptoms, as well as give advice on treatment options. Your doctor can also refer you to a specialist if necessary.
OAB symptoms can be well-controlled so that you can regain your quality of life and return to the activities and relationships, hobbies, and lifestyle you used to enjoy before OAB.

