What are kidney stones?
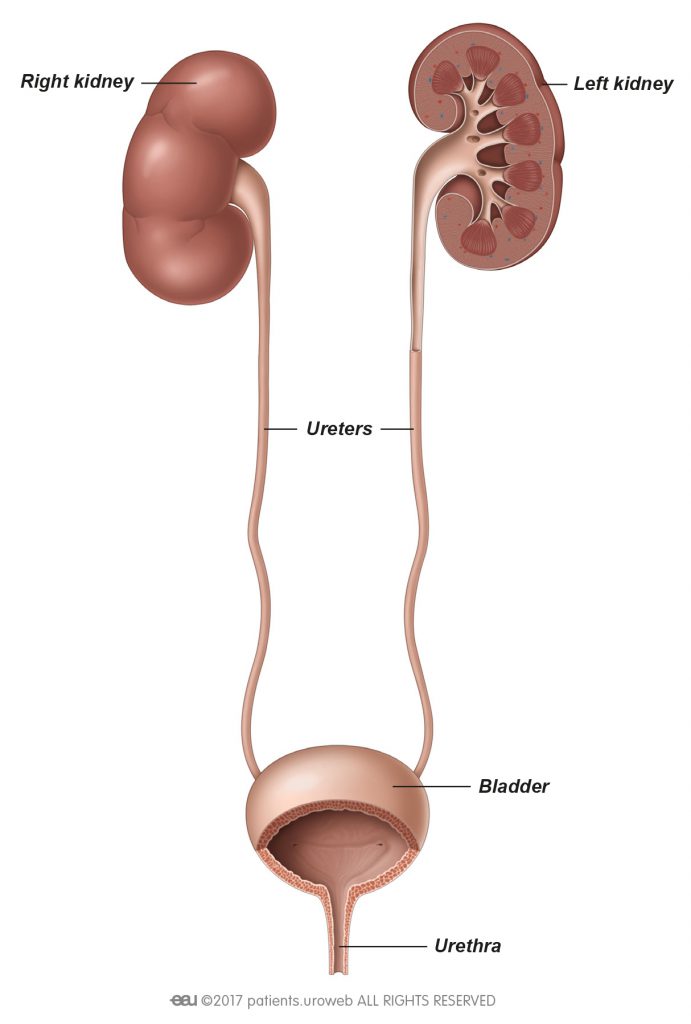
Kidney stones are hard, pebble-like objects that are made up of minerals and salts. They can affect any part of the urinary tract, from your kidneys to your bladder, and can be very painful. They are quite common, especially in people aged 30 to 60 years.
Kidney stones can be caused by not drinking enough fluids, as stones can form when urine becomes too concentrated, allowing minerals to crystallise and stick together. Other causes include a diet that is high in protein but low in fibre, excess body weight, some medical conditions, structural problems with the kidneys, inherited diseases, and certain supplements and medications.