Table of Contents
What is ablation therapy?
Ablation therapy is a type of minimally invasive surgery doctors use to destroy abnormal tissue, like small tumours, that occur with kidney cancer and prostate cancer. The goal is to remove as many cancer cells as possible. This therapy kills cancer cells by heating them or freezing them.
The following types of ablation therapy are explained here:
- Cryoablation
- High Intensity Focused Ultrasound
- Radiofrequency ablation
Who are candidates for ablation therapy?
Cryoablation
Kidney cancer
Your doctor may suggest cryotherapy if you have a small kidney tumour (less than 4 cm) and surgery is not the best option for you. This may be related to your age or any medical conditions which make surgery dangerous for you.
Prostate cancer
Cryosurgical ablation of the prostate (CSAP) is a treatment option for small localised tumour(s) in the prostate.
High Intensity Focused Ultrasound
High Intensity Focused Ultrasound (HIFU) is a treatment option for small localised tumour(s) in the prostate.
Radiofrequencey ablation
Your doctor may suggest RFA treatment if you have a small kidney tumour (less than 4 cm) and surgery is not an option for you. This may be related to your age or any medical conditions which make surgery dangerous for you.
The procedure
How is cryoablation performed?
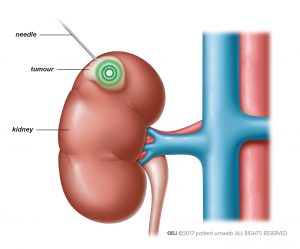
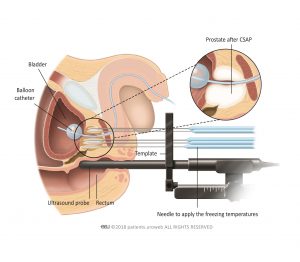
Usually cryotherapy is performed through the skin and the doctor uses ultrasound or a CT scan to guide the needle. The liquefied gas—usually liquid nitrogen or argon—reaches the tumour through the needle. (Fig. 1 and fig. 2).
Cryotherapy can also be performed during surgery. During the procedure the temperature of the organ tissue (kidney or prostate) and surrounding organs is carefully checked by thermo sensors. Cryotherapy can also be done during surgery.
Side effects
What are the side effects of cryoablation?
Cryotherapy is an effective and safe treatment, but there is a risk of tumour cells being left behind. For kidney cancer and prostate cancer, this means the tumour is more likely to come back (recurrence) than after surgery. There are also risks of complications.
Kidney cancer
For kidney cancer, the most common complications include bleeding and a build-up of blood inside the kidney, known as perinephric haematoma. During treatment, your ureter, spleen, liver, or bowel may be injured. You could also experience paraesthesia, which is a prickling or tingling sensation of the skin, around the treated area.
Prostate cancer
By using ultrasound images or (sometimes) MRI images, the cryotherapy needles can be placed very accurately. That ensures that only the tumor is treated. As a result, surrounding tissue can be spared and side effects are avoided as much as possible. Therefore, side effects are reported little.
What are the side effects of High Intensity Focused Ultrasound?
There are few side effects known. The treatment is nerve sparing so an erection remains possible. The first few days, urination is difficult, requiring a catheter. Occasionally, temporary stress incontinence occurs, i.e. (loss of a few drops of urine due to pressure, coughing or exertion).
What are the side effects of radiofrequency ablation?
While the procedure is safe, there are risks of complications. The most common complications include:
- Pain around the treated area
- Prickling of your skin or a tingling sensation (paraesthesia)
- Bleeding
- Rare need for blood transfusion
- Leaking and collection of urine around the kidney
- Ureter, spleen, liver, or bowel injury
- Infections
- Voiding problems
Follow up
After ablation therapy, follow-up visits with your doctor are scheduled every 3 months. Imaging (CT scan or MRI) is used to monitor your kidney or prostate and detect possible tumour recurrence.
Ablation therapy can be performed again if the tumour comes back or if the first treatment is unsuccessful.