Table of Contents
Artificial Compression Devices (Balloon insertion)
Artificial compression devices, also known as balloons, are a common treatment for mild to moderate stress urinary incontinence. They compress the urethra just below the bladder neck so that it can better resist the pressure of a full bladder. The goal of the balloons is to reduce urine leakage during activities such as sneezing, coughing, running or lifting.
When should I consider a balloon insertion?
Balloons can be considered in case of mild to moderate urinary incontinence. They are also recommended when other surgical treatments are not possible, or if you do not want to undergo major surgery.
The procedure
How are balloons inserted?
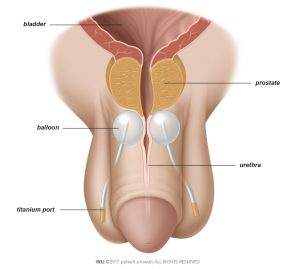
The artificial compression device consists of a balloon which can hold fluid, a small titanium port, and a tube that connects the port to the balloon. The port allows the doctor to regulate the amount of fluid in the balloon. Two balloons are inserted on either side of the urethra during a minimally-invasive procedure.
For the procedure you usually receive general anaesthesia, but in some cases you may be recommended spinal anaesthesia. First the doctor inserts a catheter to make sure that your bladder is completely empty during the surgery.
The doctor then makes an incision in the perineum. Using x-ray for guidance, the doctor places the first balloon on one side of the urethra, under the prostate. If you have had radical prostatectomy, the doctor places the balloon right under the bladder neck. This is then repeated with the second balloon on the other side of the urethra (Fig. 1).
Finally the doctor positions the titanium ports in the scrotum and connects them to the balloons. This is done so that the volume of the balloons can easily be adjusted after surgery.
How to prepare for the procedure
Before the surgery the doctor will ask for a urine sample to make sure you do not have a urinary tract infection. If you have an infection, your doctor will prescribe antibiotics before, during, and after the operation.
Your doctor will advise you in detail about how to prepare for the procedure. You must not eat, drink, or smoke for 6 hours before surgery to prepare for the anaesthesia. If you are taking any prescribed medication, discuss it with your doctor. You may need to stop taking it several days before surgery. Your doctor will advise you on when you can start taking it again.
After the procedure
How long will it take me to get back to my daily activities?
The doctor will generally remove the catheter immediately after the surgery and monitor your recovery. Usually you can leave the hospital a few days after the procedure. If you have problems urinating or there is much post void residual urine in the bladder, you may have to stay longer. The recommended length of hospital stay varies in different countries.
After any surgery, your body needs time to fully recover. It can take up to 6 weeks for the wound to heal completely. During this time you may experience pain in the pelvic area, or feel pain when you urinate. Your doctor can prescribe medication to deal with these symptoms.
Recommendations for 4-6 weeks after the surgery:
- Drink 1-2 litres every day, especially water
- Do not lift anything heavier than 5 kilograms
- Do not do any heavy exercise
- Take showers instead of baths
- Avoid thermal baths, or going to the sauna
- Adapt your diet to prevent constipation
You need to go to your doctor or go back to the hospital right away if you:
- Develop a fever
- Are unable to urinate on your own
- Have heavy blood loss or pain
- Have significant blood in the urine
- Notice the wound starts to bleed or leak transparent fluid, or it hurts