Table of Contents
Autologous fascial sling
Autologous fascial sling is a surgical treatment for stress urinary incontinence in women who cannot use a synthetic or midurethral sling.
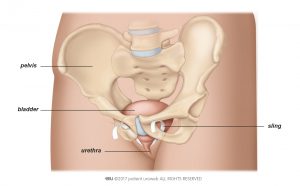
Like a synthetic midurethral sling, an autologous fascial sling is placed under the urethra (see Fig. 1a). It supports the pelvic floor muscles and helps the urethra resist increases in abdominal pressure transmitted to the bladder.
This sling is placed either at the mid urethra or nearer to the bladder, and no synthetic material is used. The sling is made from your own connective tissue, called fascia, taken from the lower belly or thigh. Removing this tissue creates additional wounds.
Autologous fascial slings and synthetic midurethral slings have similar effectiveness. Autologous fascial slings can have a slightly higher risk of complications, especially difficulty emptying the bladder.
When should I consider an autologous fascial sling?
An autologous fascial sling is a good alternative if a synthetic midurethral sling cannot be used, or if you want to avoid synthetic material. It is also an option if previous surgery for stress urinary incontinence didn’t work.
How to prepare for the procedure
Before surgery, the doctor will ask for a urine sample. This will be tested to make sure you do not have a urinary tract infection. If you have an infection, your doctor will prescribe antibiotics for you to take before, during, and after the operation.
Your doctor will advise you in detail about how to prepare for the procedure. If you need general anaesthesia, you must not eat, drink, or smoke for 6 hours before the surgery. If you take any prescribed medication, discuss it with your doctor. You may need to stop taking medication several days before surgery. Your doctor will advise you on when you can start taking it again.
The procedure
How is an autologous fascial sling implanted?
You will typically be unconscious (general anaesthesia) for this procedure. Spinal anaesthesia can also be used to block nerve response to pain.
Steps:
- The bladder is emptied. The surgeon will insert a catheter to make sure that your bladder is completely empty during surgery.
- Connective tissue is harvested. A cut, typically horizontal, is made a few centimetres long in the lower belly. A strip of fascia is taken from the rectus muscle. This strip is typically more than 8 cm long and 1.5 to 2 cm wide. Then the fascia is closed.
- The sling is placed. The surgeon makes a small cut in the front of the vaginal wall. The fascial strip is placed under the urethra near the bladder. The two ends of the sling are brought to the lower belly area using a special instrument and attached just above the pubic bone (retropubic route). The sling is secured using suture material.
- The inside of the bladder is examined (cystocopy). The surgeon will look through your urethra into your bladder using a very small camera to rule out injury to the bladder.
After the procedure
How long will it take me to get back to my daily activities?
You can usually leave the hospital two to three days after implantation of a an autologous fascial sling. You may have to stay in the hospital longer if you are unable to urinate or your bladder is not emptying completely. The recommended length of hospital stay varies in different countries.
Complete recovery from surgery may take up to 6 weeks. During this time, you may have pain in the pelvic area or when you urinate. Your doctor can prescribe medication for these symptoms.
Recommendations for 4–6 weeks after surgery:
- Drink 1–2 litres every day, especially water
- Do not lift anything heavier than 5 kilograms
- Do not do any heavy exercise
- Take showers instead of baths
- Avoid thermal baths or going to the sauna
- Adapt your diet to prevent constipation
- Avoid vaginal penetration
Call your doctor or go back to the hospital right away if you:
- Develop a fever
- Are unable to urinate
- Have heavy blood loss or pain
- Notice the wound starts to bleed or leak clear fluid
- Notice the wound hurts

