Orchidectomy
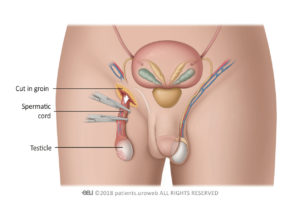
An orchidectomy (unilateral), is an operation to remove one testicle. It is carried out under a general anaesthetic, which means you are asleep during surgery. During surgery, a small incision is made into the groin region on the affected side and the testicle is removed. The scrotum is not cut. The cancerous testicle will then be sent to a laboratory to be analysed.
After Surgery
- A dressing will cover the incision site on the groin which can be removed after 24 hours. Stitches (sutures) will dissolve but may take a few weeks to disappear.
- You can have a bath or shower after 24 hours, but do not rub soap on the wound area. The area should be dried by gently patting it with a clean towel.
- The groin and scrotal area will feel bruised and swollen after the operation. It is better to wear close fitting underwear, such as briefs or ‘Y’ fronts or a scrotal support rather than boxer shorts. This will help the bruising settle.
- Painkillers should be taken as prescribed on a regular basis.
- Although this is a minor operation, you should reduce strenuous activity for the first week but should be able to return to work within a few weeks.
- Occasionally a collection of blood may form around the wound (haematoma) or it may become infected. You should seek medical advice if the operation site becomes very red or sore which could be signs of infection.
- You should only start driving when you are able to perform an emergency stop without hesitation.
- Sexual activity can begin after two weeks if it feels comfortable to do so.
Having an orchidectomy should not affect your ability to have an erection, but the stress associated with a potential diagnosis of cancer may affect sexual performance.
Prosthetic (artificial) testicle
A prosthetic or artificial testicle is a silicone implant which will resemble a normal testicle. It can be inserted at the time of orchidectomy or if you are unsure that you want one, after your treatment has finished. Once inserted, the neck of the scrotum is sealed with stitches to prevent it from moving up into the groin.
Some possible problems with implants may include:
- The cosmetic result may vary. For example the artificial testicle may not exactly match the size of the normal testicle that remains on the other side.
- Scar tissue can form around the implant inside the scrotum. This can sometimes cause a thickening of tissue which may in turn cause discomfort.
- Although exceptionally rare, rupture of the implant can occur due to vigorous activities such as contact sport, cycling or physical contact including sexual intercourse.
- Sometimes the implant may move out of its original position.
- A prosthetic testicle will not react to temperature like a normal one and will stay the same size.
- If you need chemotherapy treatment after orchidectomy an artificial implant may increase the risk of infection due to a lowered immune system.
What happens next?
The MDT (Multi-Disciplinary-Team) Process
An MDT is a group of medical experts who are managing your care. When the results of surgery, blood tests and scans are available, they will make a recommendation about any further treatment that you may need. Several options may be recommended for further treatment, and these will be discussed with you.
The following treatment(s) may be recommended after orchidectomy depending on the stage of the cancer.
Stage 1
| Surgery | Chemotherapy | Radiotherapy |
|
Orchidectomy |
A short course of chemotherapy may be recommended depending on the risk of testicular cancer coming back. Alternatively, a programme of surveillance may be suggested to check for cancer on a regular basis. If there is any evidence that cancer has returned chemotherapy will be given to cure it. For early-stage testicular cancer men may be given both options and asked to decide which they would prefer. In this situation there is no right or wrong answer. https://www.youtube.com/watch?v=eAz-rBfO0lQ
|
For seminoma only depending on risk factors. Used to kill cancer cells in the lymph nodes at the back of the abdomen. |
Stage 2
| Additional Surgery | Chemotherapy | Radiotherapy |
|
If a non-seminoma cancer is present or some blood tumour markers are high, lymph nodes in the abdomen may be removed by an operation called a Retro Peritoneal Lymph Node Dissection (RPLND).
|
Yes
|
This is only used for seminoma and is used to kill cancer cells in the lymph nodes at the back of the abdomen. A short course of chemotherapy may also be given. |
Stage 3
| Additional Surgery | Chemotherapy | Radiotherapy |
|
Tumours that have spread to other areas such as the abdomen will be removed by an operation called a Retro Peritoneal Lymph Node Dissection (RPLND) typically after chemotherapy. Cancer which has spread to other areas of the body such as the liver or lungs will also be surgically removed.
|
Yes
|
No |