What are congenital malformations of the urinary tract (“urinary tract differences”)?
A small number of babies, while growing in the womb, may develop some differences in their urinary system (the organs in the body that produce and carry away urine). These differences are known as “congenital malformations of the urinary tract”.
Broken down, this medical term means:
- Congenital – a condition that develops during development in the womb
- Malformation – where an organ develops differently than usual
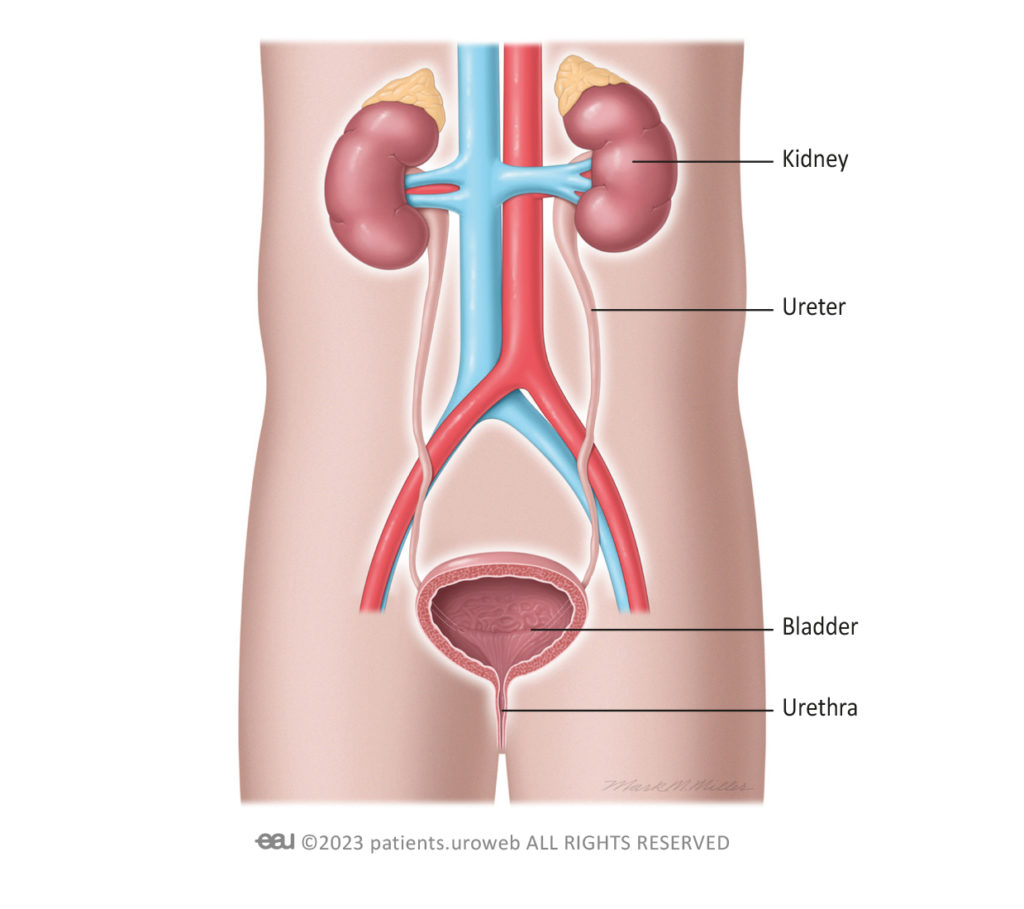
- Urinary tract – consisting of the kidneys, the ureters (the tubes that connect the kidneys to the bladder), the bladder, and the urethra (the wee tube that carries urine from the bladder and out of the body)
Throughout this website, we refer to congenital malformations of the urinary tract as “urinary tract differences”.
Although urinary tract differences are rare, the most common ones are:
- Hydronephrosis (pronounced ‘hi-dron-eff-roe-sis’)
This condition is where one or both kidneys swell up due to the build up of urine. This happens if urine is unable to flow from the kidney (or both kidneys) to the bladder and is sometimes caused by a blockage or a urinary infection. - Ureteral duplication (pronounced ‘yur-eet-eral dew-plik-ay-shun’), also called duplex kidney
This is where one or both kidneys have an extra ureter tube connecting down to the bladder, rather than one ureter connecting the kidney to the bladder. - Ureterocele (pronounced ‘yur-reet-ero-seel’)
This is where the lower part of the ureter becomes enlarged and forms a balloon-like structure inside the bladder. - Ectopic ureter (pronounced ‘ek-top-ik yur-eet-er’)
This describes a condition where the upper part of the ureter attaches incorrectly elsewhere in the urinary tract or bladder. - Vesicoureteral reflux (pronounced ‘vessy-co-yur-eet-er-ral ree-flux’), also called VUR
VUR happens when urine flows backward from the bladder, back up into one or both ureters, and sometimes even into the kidney.
These urinary tract differences may be found during one of the ultrasound scans that are carried out throughout your pregnancy. Being told your unborn child or, if the condition is diagnosed after birth, your newborn, has any kind of medical problem can be a worrying time, but it’s important for you to know that most children born with urinary tract differences don’t experience any symptoms or urinary problems at all.
Urinary tract differences can occur due to unexplained changes in genes that happen while a baby is developing in the womb. In rare cases, they can be inherited (passed down) from the parents.
Sometimes, urinary tract differences can occur alongside congenital malformations (differences) in other parts of the body. For instance, there are over 500 medical conditions that are linked to urinary tract differences.
Medical tests, such as regular ultrasounds carried out during pregnancy, can identify these potential differences early on so that they can be monitored and treated, if necessary. If your child is found to have a difference in the structure of their urinary tract, a team of specialist healthcare professionals will support you and your family to ensure your child receives the best possible care and treatment for their individual needs.