Table of Contents
About the urinary system
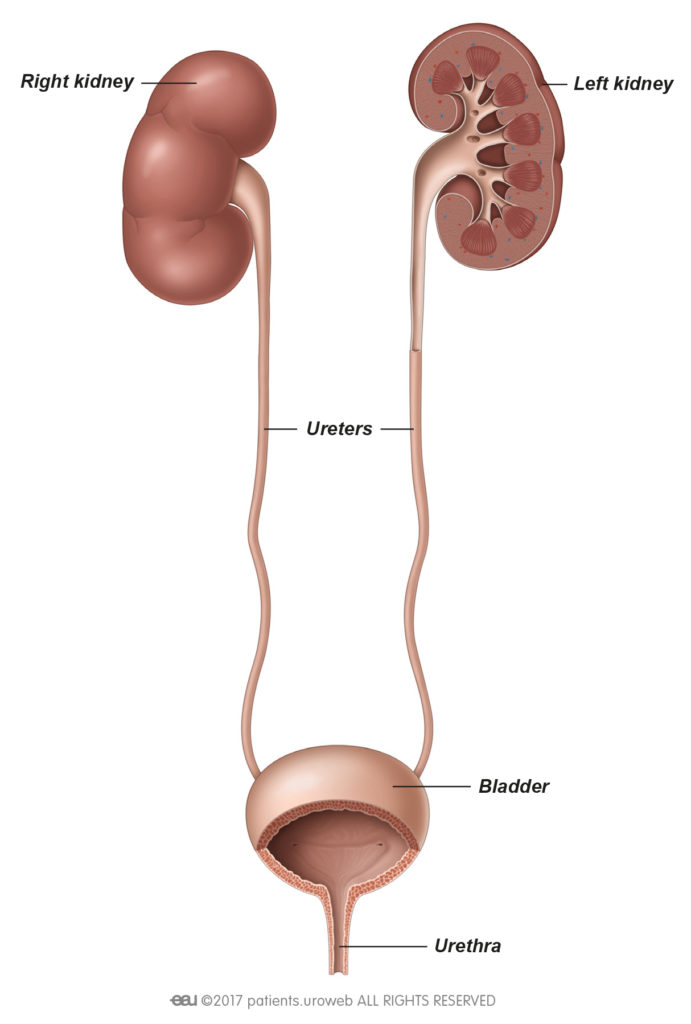
What is the urinary system?
Your urinary system includes your kidneys, ureters, bladder, and urethra. Together, these organs filter, store, and remove waste from your body.
What does the urinary system do?
Your urinary system acts like a filter inside your body. A series of tubes and ducts connected to your blood vessels remove toxins and waste products with your urine.
Urinary tract infections
What are urinary tract infections?
There are several conditions that can affect the different organs that make up your urinary system, but the most common problems are caused by infections. Here you can find more information about the symptoms, tests, treatments, and prevention of the most common urinary tract infections, or UTIs.
Cystitis
What is cystitis?
Cystitis is the medical term for inflammation of the bladder. It comes from the Latin word “cystis” which means bladder-like bag, and “-itis” which is used in medicine to describe diseases that involve inflammation.
Watch this video about cystitis, the most common UTI.
Most of the time, the inflammation is caused by bacteria inside the bladder called Escherichia coli, commonly shortened to E.coli. It isn’t always obvious how E.coli enters the bladder, but some known risk factors include:
- having sex
- wiping your bottom from back to front after going to the toilet
- using a diaphragm for contraception
Constipation and not drinking enough water can aggravate urinary problems and are also risk factors for cystitis.
Although anyone can develop cystitis, it is more frequently experienced by women. Almost half of all women will experience at least one episode of cystitis in their lifetime. Nearly 1 in 3 women will have had at least one episode of cystitis by the age of 24.
While cystitis can be painful, it is more of a nuisance than a serious health problem and usually clears on its own within a few days.
What are the common symptoms?
Cystitis symptoms usually appear suddenly, rather than gradually, and can make you feel unwell. The most common symptoms include:
- pain, burning, or a stinging sensation when you pass urine (called dysuria)
- pain in the lower abdomen
- feeling the need to urinate more than normal
- frequently passing a small amount of urine
- blood in your urine (called haematuria)
- dark, cloudy, or strong-smelling urine
Mild cases often get better on their own, but if you have had symptoms for more than 3 days, talk to your doctor. Some of the symptoms can be similar to other conditions, so it is important to get a proper diagnosis if you are not sure whether you have cystitis.
What tests and checks are available?
Urine test
Your doctor will ask you about your symptoms and discuss your medical history, including any medication you take. Your abdomen and back will be examined and you will be asked for a sample of urine to test for an infection. This may be sent to a laboratory for further testing depending on the facilities available at your local clinic.
Ultrasound
In some cases, your doctor may perform an ultrasound of your bladder and kidneys to check for other possible causes of your symptoms.
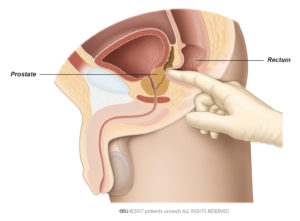
Prostate check (men only)
A prostate check, or digital rectal examination, is a quick and simple test to see if your symptoms might be caused by a prostate problem. It involves your doctor inserting a gloved and lubricated finger into your back passage (rectum) to feel your prostate.
We realise this might seem embarrassing, but the examination is over very quickly. You may be aware of some pressing and get a brief urge to pass urine, but the examination itself is not usually painful.
What treatments are available?
Home remedies
If your symptoms are mild, you may find relief from the following:
- over-the-counter painkillers, such as paracetamol or ibuprofen
- drinking plenty of water
- avoiding sex until you’re feeling better
Some people find drinking cranberry juice or using products that lowers the acidity of their urine, such as sodium bicarbonate or potassium citrate, helps to reduce their symptoms, but there is a lack of evidence to confirm how effective these treatments are.
Antibiotics
If your symptoms don’t go away, then you may need antibiotics to clear the infection. In this instance, your doctor will prescribe you tablets or capsules to take either as a “single shot” meaning one dosage only or 2 to 4 times a day for 3 days or more. Antibiotics usually start to work quickly, and you should expect to start feeling better within a few days. It is important to make sure you take the entire course of antibiotics recommended by your doctor, even if you start feeling better sooner.
Most people don’t get any side effects from antibiotic treatment, but make sure you read the medicine information leaflet to familiarise yourself with the known side effects.
What happens if cystitis comes back?
Some women find they have repeated bouts of cystitis, referred to as recurrent cystitis. It is not always clear why people get recurrent cystitis, but if this happens, talk to your doctor about a referral to a urologist.
A urologist may perform further tests, such as an internal examination (for women) or arrange for you to have a cystoscopy. This is a procedure to look inside the bladder using a thin device called a cystoscope.
Your urologist will also discuss possible longer-term treatments with you, which may include vaginal oestrogen (for women), immunostimulants or continuous antibiotics.
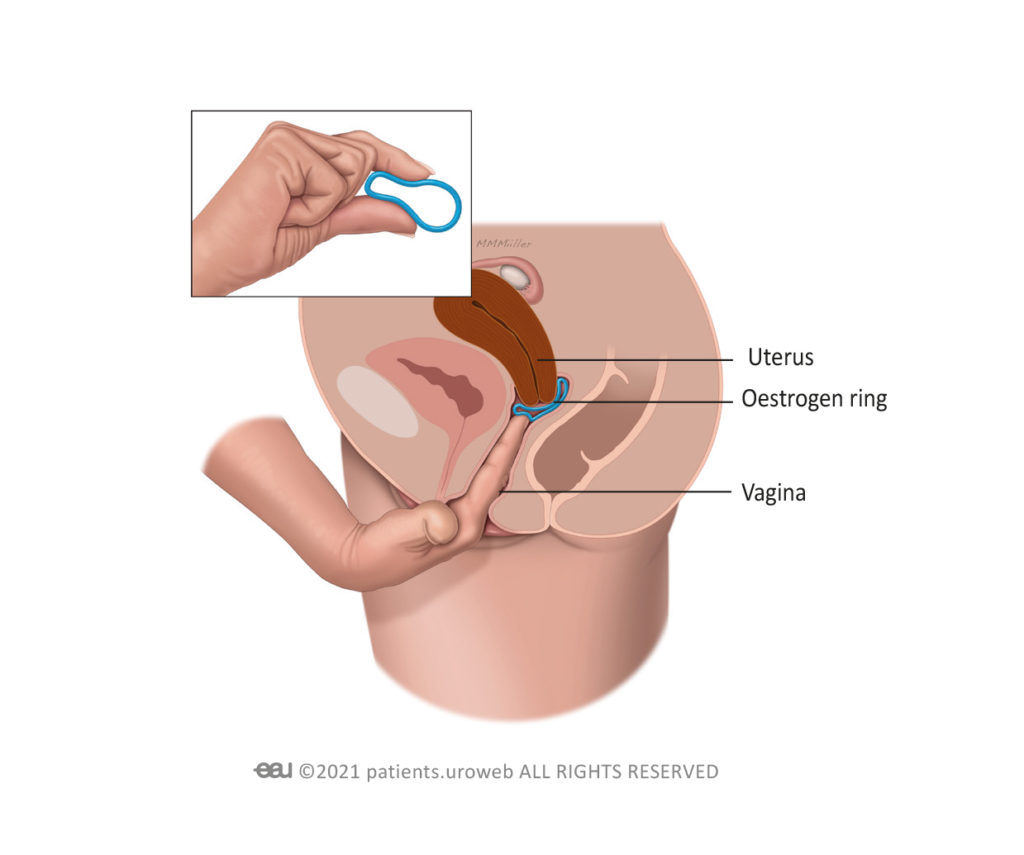
Vaginal oestrogen (women only)
Post-menopausal women who have recurrent episodes of cystitis may be prescribed vaginal oestrogen. This is usually taken as a tablet that you need to insert into your vagina at night twice a week, or as a soft ring that is inserted into the vagina and stays in place for 3 months at a time.
Immunostimulants
Immunostimulants are medications taken by mouth that act by stimulating your body’s natural defences or immunity against urinary infections, particularly those that affect the bladder causing cystitis.
Bladder instillations
Intravesical therapy is the medical term for a bladder instillation, sometimes also called a bladder wash. It is a treatment where a liquid drug is administered into the bladder to coat the lining of your bladder with a protective layer which can help reduce your symptoms.
Bladder instillation involves having a catheter inserted into your bladder via your urethra. Once your bladder has been filled with the liquid drug you will be advised not to pee for a specified amount of time to allow the drug to work.
Food supplements
D-Mannose is a naturally occurring sugar with anti-inflammatory properties that can be bought in both powder and tablet form from many health food shops. D-Mannose might help to heal the bladder and calm the inflammation.
Stand-by or continuous antibiotics
Your doctor may prescribe you a low dose of antibiotics which you will need to take for several weeks or months to help clear the infection. Alternatively, if you suffer from recurrent cystitis after having sex, your doctor may be able to prescribe you antibiotics to take after intercourse to help prevent a cystitis flare up. Although it can be embarrassing talking about sex with your doctor, if you think your cystitis is triggered by having sex, an open discussion can help you get the treatment you need.
Is there anything else that can help?
Unfortunately, there is limited evidence that lifestyle changes really help to prevent cystitis, however, some people find the following tips can help reduce recurrent cystitis:
- drinking plenty of water throughout the day to help flush out the bacteria
- wiping your bottom from front to back after going to the toilet
- going to the toilet when you feel the urge to urinate, rather than holding it
- urinating shortly after sex
- taking showers instead of baths and washing yourself every day
- avoiding products that irritate your genital area, such as soap, deodorant sprays, powders, or spermicide gels
Pyelonephritis
What is pyelonephritis?
Pyelonephritis is a bacterial infection of kidneys that usually starts in the lower parts of the urinary tract. Bacteria in the urethra spreads to the bladder and then up to one or both kidneys via the ureters. If you have a kidney infection, it is important to get prompt medical attention. If not treated, a kidney infection can cause serious health problems including damage to your kidneys, or septicaemia.
Like cystitis, pyelonephritis is more frequently experienced by women, but men can also experience kidney infections. Some people have a higher risk of developing pyelonephritis, including:
- pregnant women
- patients with diabetes or immune disorders
- patients with stones in their urinary tract
- patients with an abnormality of urinary tract
What are the common symptoms?
Signs and symptoms of a kidney infection can include:
- a fever (temperature above 38°C or 100.4°F) or chills
- nausea and vomiting
- back, side (flank) or groin pain
- pain, burning, or a stinging sensation when you pass urine (called dysuria)
- pain in the lower abdomen
- feeling the need to urinate more than normal
- blood or pus in your urine (called haematuria)
- dark, cloudy, or strong-smelling urine
Severe kidney infections can lead to life-threatening complications, so it is important that you see a doctor as soon as possible.
What tests and checks are available?
Urine test
Your doctor will ask you about your symptoms and discuss your medical history, including any medication you take. Your abdomen and back will be examined and you will be asked for a sample of urine to test for an infection. This may be sent to a laboratory for further testing depending on the facilities available at your local clinic. The results will confirm if there are bacteria, red or white blood cells in your urine and help your doctor decide on the best treatment option for you.
You may also be asked to provide a urine sample for a culture to find out the specific bacteria causing the infection.
Ultrasound
Your doctor may perform or refer you for an ultrasound of your bladder and kidneys to check for other possible causes of your symptoms, such as cysts, tumours, or an obstruction.
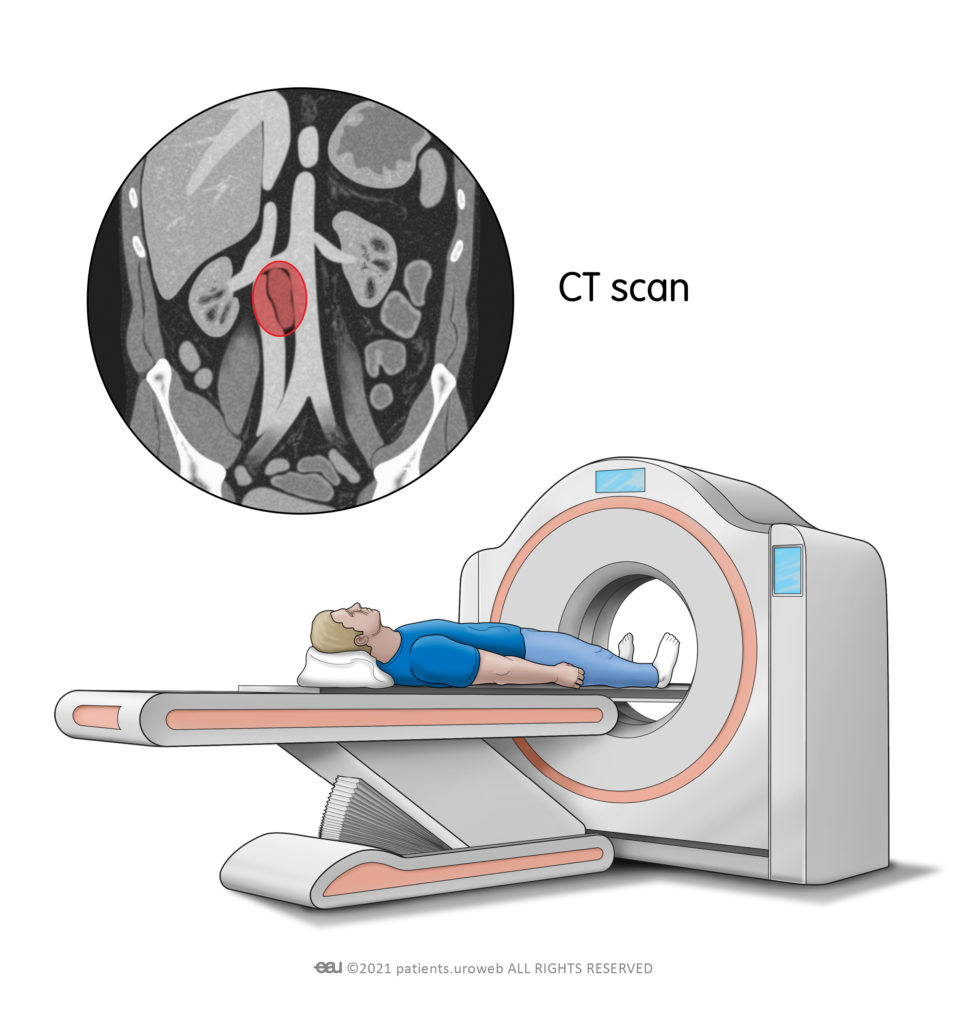
CT scan
In some cases, your doctor may arrange for you to have a computerized tomography scan, or CT scan. A CT scan provides a more detailed image of your organs than normal ultrasound.
During the CT scan, you will be asked to lie on the scanner bed. The bed moves forwards and backwards through the hole of the scanner. You will be able to communicate with the radiographer the whole time.
Prostate check (men only)
A prostate check, or digital rectal examination, is a quick and simple test to see if your symptoms might be caused by a prostate problem. It involves your doctor inserting a gloved and lubricated finger into your back passage (rectum) to feel your prostate.
We realise this might seem embarrassing, but the examination is over very quickly. You may be aware of some pressing and get a brief urge to pass urine, but the examination itself is not usually painful.
What treatments are available?
Antibiotics
The first-line treatment for kidney infections is antibiotics. The antibiotic you are prescribed, and the course of treatment, will depend on any medical conditions you have, and the specific bacteria found in your urine or blood tests. Depending on the severity of your infection and symptoms, you may also be prescribed pain killers and fever reducing drugs.
Usually, you can expect your symptoms to start to clear up within a few days of treatment. But it is important to make sure you take the entire course of antibiotics recommended by your doctor, even if you start feeling better sooner.
Your doctor might recommend you have a further urine sample tested to ensure the infection has cleared. If the infection has not cleared up, you may need to take another course of antibiotics.
Hospitalisation
If your kidney infection is severe, your doctor might recommend you receive treatment as an inpatient at a hospital. Treatment might include antibiotics and fluids that you receive through a vein in your arm, called an intravenous infusion. Your length of stay and treatment will depend on how severe the infection is and your overall health.
Surgery
If your urine flow is blocked by a stone or structural problem within your urinary tract, your doctor will recommend surgery to put a soft plastic tube, called a stent, in place. This will allow urine to drain from your kidneys to your bladder. The procedure is called ureteric stenting.
You will be given an anesthetic to numb the area around your pelvis so you will not feel any pain during the procedure, but you may feel some pressure.
This short video explains the procedure in more detail.
What happens if pyelonephritis comes back?
If you keep getting kidney infections, it may be due to an underlying medical problem. If this happens, talk your doctor about further investigations and possible longer-term treatments.
Unfortunately, there is limited evidence that lifestyle changes really help to prevent pyelonephritis, however, some people find the following tips can help reduce recurrent episodes:
- drinking plenty of water throughout the day
- wiping your bottom from front to back after going to the toilet
- going to the toilet when you feel the urge to urinate, rather than holding it
- urinating shortly after sex
- taking showers instead of baths and washing yourself every day
- avoiding products that irritate your genital area, such as soap, deodorant sprays, powders, or spermicide gels
Catheter-associated urinary tract infections
What are catheter-associated UTIs?
A urinary catheter is a tube inserted into the bladder through the urethra to drain urine. They are commonly used in hospitals before or after surgical procedures and in people who have bladder function problems.
Catheter-associated UTIs occur when bacteria enter the urinary tract through the catheter, causing an infection.
What are the common symptoms?
The symptoms of a catheter-associated UTI are similar to typical urinary infections:
- a fever (temperature above 38°C or 100.4°F) or chills
- pain in the lower abdomen or lower back
- feeling the need to urinate more than normal
- blood in your urine (called haematuria)
- dark, cloudy, or strong-smelling urine
- urine leakage around your catheter
- unexplained fatigue
- vomiting
What tests and checks are available?
Urine test
Your doctor will ask you about your symptoms and discuss your medical history, including any medication you take. Your abdomen and back will be examined and you will be asked for a sample of urine to test for an infection. This may be sent to a laboratory for further testing depending on the facilities available at your local clinic. The results will confirm if there is bacteria or blood in your urine and help your doctor decide on the best treatment option for you.
You may also be asked to provide a urine sample for a culture to find out the specific bacteria causing the infection.
Prostate check (men only)
A prostate check, or digital rectal examination, is a quick and simple test to see if your symptoms might be caused by a prostate problem. It involves your doctor inserting a gloved and lubricated finger into your back passage (rectum) to feel your prostate.
We realise this might seem embarrassing, but the examination is over very quickly. You may be aware of some pressing and get a brief urge to pass urine, but the examination itself is not usually painful.
What treatments are available?
Antibiotics
Your doctor will prescribe you antibiotics, but the exact dose and course of treatment will depend on any existing medical conditions you have, and the specific bacteria found in your urine. Depending on the severity of your infection and symptoms, you may also be prescribed pain killers and fever reducing drugs.
Usually, you can expect your symptoms to start to clear up within a few days of treatment. But it is important to make sure you take the entire course of antibiotics recommended by your doctor, even if you start feeling better sooner.
Your doctor might recommend you have a further urine sample tested to ensure the infection has cleared. If the infection has cleared up, you may need to take another course of antibiotics.
Hospitalisation
If you are an outpatient and your infection is severe, your doctor might recommend you receive inpatient care at a hospital. Your length of stay and treatment will depend on how severe the infection is and your overall health. Treatment might include antibiotics and fluids that you receive through a vein in your arm, called an intravenous infusion.
If you are already receiving treatment in hospital, you may need to stay in hospital longer than expected to make sure the antibiotics are working, and your infection does not worsen. Catheter-associated UTIs are dangerous because they can lead to severe kidney infections, so it is important that you listen to your doctors and the nursing staff.
What happens if I keep getting infections?
You will only be given a urinary catheter if your doctor believes it is necessary and it will be removed as soon as possible. However, catheter-associated UTIs are one of the most common hospital-related infections, so many healthcare organisations have plans in place to help reduce the number of infections and recurrences.
You will only be given a urinary catheter if your doctor believes it is necessary and it will be removed as soon as possible. However, catheter-associated UTIs are one of the most common hospital-related infections, so many healthcare organisations have plans in place to help reduce the number of infections and recurrences. Other prevention measures include:
- keeping the drainage bag below your bladder
- emptying the drainage bag several times per day
- ensuring there are no kinks in the catheter tube
- changing the catheter at least once per month
Asymptomatic bacteriuria
What is asymptomatic bacteriuria?
Asymptomatic bacteriuria is the medical term for bacteria in the urine without causing any symptoms. In asymptomatic bacteriuria, bacteria colonise the urinary tract. So, although bacteria are present in the bladder, it is not actually causing inflammation or infection, which is why none of the symptoms of a urinary tract infection are experienced.
What are the common symptoms?
Asymptomatic bacteriuria does not cause any symptoms.
If you have symptoms, such as pain, burning, or a stinging sensation when you pass urine or dark, cloudy, or strong-smelling urine then you might have a urinary tract infection.
How would I know if I had asymptomatic bacteriuria?
Some people have a higher risk of developing asymptomatic bacteriuria than others and it is more common in men and women over the age of 65, especially those who are in long-term care, such as care homes. But it can also occur in people with diabetes, pregnant women, and in children. If you are at risk, then your doctor may perform tests or checks to see if you have the condition.
Should I be concerned about asymptomatic bacteriuria?
Asymptomatic bacteriuria does not usually require treatment. This is because the lack of symptoms suggests no inflammation or infection are present, and the bacteria may clear spontaneously over time. If you are not at risk of developing asymptomatic bacteriuria, then the condition rarely causes serious problems.
If you are pregnant or undergoing certain urological procedures, then you will be tested for asymptomatic bacteriuria due to the risk of urinary infections.
What tests and checks are available?
Urine test
A positive urine culture is the only way of diagnosing asymptomatic bacteriuria. Your doctor will ask for a sample of urine which will be sent to a laboratory to confirm if there are bacteria in your urine.
Cystoscopy
In some cases, if a certain bacterium is detected, your doctor may arrange for you to have a cystoscopy. This is a procedure to look inside the bladder using a thin device called a cystoscope.
What treatments are available?
You doctor may also prescribe you antibiotics before undergoing a procedure involving your urinary tract or prostate if bacteria is detected in your urine. It is important to make sure you take the entire course of antibiotics recommended by your doctor or surgeon.
What happens if asymptomatic bacteriuria comes back?
Studies have found that in older adults, asymptomatic bacteriuria can spontaneously clear on its own, but it also often comes back or persists.
The following practices may help prevent the colonisation of bacteria:
- drinking plenty of water throughout the day
- wiping your bottom from front to back after going to the toilet
- urinating shortly after sex