Table of Contents [hide]
This page provides you with essential information about percutaneous nephrolithotomy (PCNL). It also contains an animation that shows what happens when you undergo a PCNL.
PCNL is used most often when kidney stones are too difficult to reach, too large, too numerous, or too dense to be treated by shock wave lithotripsy or ureteroscopy.
The PCNL procedure
- PCNL is typically performed with the patient under general anaesthesia.
- During this procedure, a small tube called a catheter is placed in the bladder. The bladder catheter drains urine from the bladder and remains in place with the use of a balloon.
- Another catheter is placed into the ureter. A contrast, or dye, may be infused through this catheter to provide a better view and show the exact stone location. This facilitates access to the kidney while your urinary tract is visualised using x-rays or ultrasound.
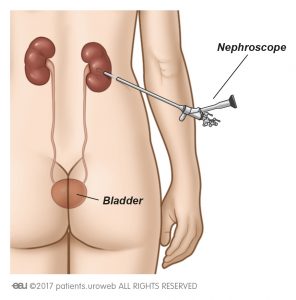
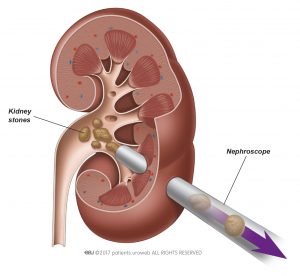
- Once the stone is located, the kidney’s collecting system is accessed using a thin needle and a so-called guidewire is placed. The guidewire permits safe access for the nephroscope, a thin tube-like instrument used for viewing the inside of the kidney.
- The access route is carefully opened until access with the nephroscope is possible.
- Some stones can directly be removed using a grasper. This is called nephrolithotomy. Larger stones need to be broken up using a device like a laser before they can be removed. This is called nephrolithotripsy.
- After all stones are removed, your surgeon will use contrast material to confirm that no stones or fragments were left behind in the kidney. When the contrast material moves easily through the bladder, this means that there are also no stones in the ureter. The ureter is the part which connects the kidney to the bladder.
- In some patients, a temporary small tube called a ‘double-J stent’ may be placed to ensure that swelling does not block the drainage of urine. The JJ-stent remains in place by J-shaped curls in both the kidney and the bladder.
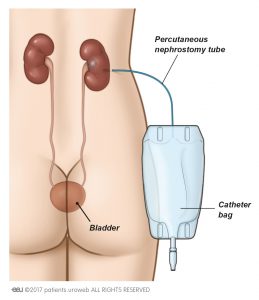
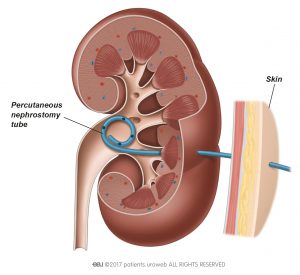
- At the end of the procedure, a drainage catheter, called a ‘nephrostomy’, may be placed.
How to prepare for the PCNL procedure
Always ask your doctor about the treatment-steps and any special instructions. These can differ by hospital and country.
Instructions may include:
- When to stop certain medications, such as blood thinners.
- When to empty the bladder before the procedure.
- When to arrange pain medication after the procedure (if necessary). Discuss this early with your nurse and/or doctor.
- Arranging a ride home after your hospital discharge.
- Not to eat, drink, or smoke for approximately 6-8 hours before the procedure to prepare for the anaesthesia.
Before surgery, someone from your health care team, usually the anaesthesiologist, will decide which method of anaesthesia is appropriate for you.
You may be asked to give a urine sample before the procedure to test for a urinary tract infection.
Medical Team
In addition to the doctor and nurses in the hospital who are responsible for your treatment, it is important that your general practitioner and other caregivers including family and friends are informed about your treatment.
Support and questions
It can help and make you feel more comfortable if your partner, relatives or friends have read the information regarding PCNL. Write down all your questions to remind you of any important points you need to discuss with your doctor or nurse.
Let someone accompany you to an appointment to help you remember any questions you may need to ask.
The PCNL operation
This animation shows what happens when you undergo a PCNL.
What to expect after the PCNL procedure
Depending on the hospital, you will either go to the recovery room or to your own room after the treatment. Your blood pressure, heart rate and pain will be checked regularly. Ask your nurse about visiting hours for friends and relatives.
- Double-J stent: In some patients, a temporary small tube, called a JJ-stent, is placed in the ureter (see Fig. 1). This stent helps urine flow to the bladder if the ureter is swollen after the procedure. The JJ-stent can be removed before your hospital discharge or shortly after at a separate appointment with your doctor.
- Urinary catheter: After surgery you may also have a catheter to drain urine from the bladder. This tube is placed through the urethra into the bladder. You will also be given fluids to help you stay hydrated. The urinary catheter is usually removed shortly (within a couple of days) after the procedure.
- Nephrostomy tube: If a nephrostomy tube is placed during surgery, there is a small possibility that you have it for a short while after hospital discharge. The tube exits your skin at the site of the surgical opening and drains urine and blood (from surgery) directly from your kidney into a drainage bag (see figure 2b). The tube is typically removed several days after surgery.
You can leave the hospital after a few days if you are able to empty your bladder sufficiently and you have no fever or not too much pain.
You may feel mild to moderate pain in your lower abdomen, and you may have a strong urge to urinate. These symptoms are usually caused by the inserted catheter(s) and/or the double-J stent. Medication is available to treat these symptoms—do not hesitate to ask.
What to expect back home
Your doctor or nurse will provide discharge instructions for rest, driving, and physical activities after PCNL.
- Double-J stent: If a JJ-stent was placed during the procedure and was not taken out before your hospital discharge, your doctor will tell you when it needs to be removed. This can take anywhere from several days to a few weeks.
- Nephrostomy tube: If a nephrostomy tube was placed during surgery, you may have it for a short while. Taking care of your nephrostomy tube is important to ensure proper healing of your kidney. Your doctor will give you the necessary instructions.
Pain after surgery
Because instruments were inserted into your urinary tract, you may have several urinary symptoms for some time after surgery. These problems usually disappear in a few weeks.
Symptoms may include:
- A mild burning feeling when urinating
- Small amounts of blood in the urine
- Mild discomfort in the bladder area or kidney area when urinating
- Need to urinate more frequently or urgently
- Pain resulting from an internal abrasion that needs time to heal
- Try to drink fluids often, but in small quantities. Sometimes a temporary blood clot can cause pain (colic).
If the pain remains despite pain medicine, contact the hospital or your doctor.
What can I do the first week after surgery?
- Try to drink enough fluids: 1.5 litres daily (in small quantities) throughout the day to help urine flow and small stone fragments to drain spontaneously.
- Eat more vegetables and less meat to have a softer stool—if you do not have to squeeze during the toilet visit, it will help the inner healing process.
- Give your body a rest during the first week after the procedure. Be careful lifting heavy objects and doing strenuous exercises.
When should I call the hospital or my general practitioner?
When you have:
- Fever higher than 38.5 degrees
- Nausea and vomiting
- Chest pain and difficulty breathing
- Large amounts of blood in your urine, and it does not go away with rest or hydration
- Severe pain in your side, despite taking pain medicine
- A serious burning sensation (not mild) when urinating
- Inability to urinate
- If a nephrostomy tube was placed, persistent urinary leakage from the nephrostomy site
Tell your doctor right away if bleeding or pain is severe or if problems last longer or worsen after you leave the hospital.
Your doctor may prescribe an antibiotic to treat or prevent an infection or relieve your pain. You should report any signs of infection––including severe pain, chills, or fever—to your doctor right away.
Follow-up after PCNL
A follow-up appointment will be scheduled with you prior to discharge from the hospital. This appointment might be necessary for:
- Laboratory results
- Ultrasound or X-rays to check for stones
- Removal of a double-J stent or nephrostomy tube
Laboratory results
The removed stone will be sent to the laboratory to determine its composition. This may take several weeks. Based on the laboratory results, along with blood and urine tests taken before treatment, your doctor can determine whether you are at high risk of forming new stones (recurrence).
Ultrasound or X-rays
Your doctor may also do an ultrasound or X-rays to check for any stones that may be left and to make sure that there is good passage of urine from the kidney to the bladder.
Removal of a JJ-stent or nephrostomy tube
A JJ-stent and/or a nephrostomy tube are usually removed in a brief procedure in the urologist’s office. This generally takes a few minutes to perform.
What if the doctor suspects that I have a high risk of forming new stones?
If the results show you have a high risk of forming more stones, your doctor will do a metabolic evaluation. This is a series of blood and urine tests to determine the possible causes of your stone formation. Depending on the test results, your doctor will recommend preventive measures or further tests. Besides changes in your lifestyle, you may also be advised to take medication that reduces the risk of stones recurring. Generally, the medication will cause few or no side effects.
Changes in your lifestyle
Even if you have a low risk of forming another stone, your doctor and nurse will advise you to make some lifestyle changes.
Lifestyle changes may include:
- Increase in fluid intake (drinking advice): 2.5-3.0 L/day to neutralize the pH of your urine
- Adopting a balanced diet, with less meat and alcohol and more vegetables and fibre, to have healthy calcium levels and less animal protein
- Maintaining a healthy weight (normal body mass index) and adequate physical activity