Table of Contents [hide]
About prostate cancer
What is the prostate, and what does it do?
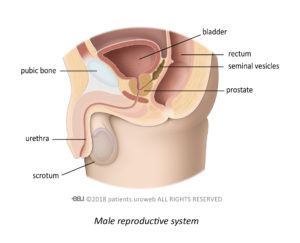
The prostate is a small gland that forms part of your reproductive system. It is about the size of a golf ball and surrounds the tube that empties urine from your bladder, called the urethra.
The prostate makes a thick white fluid that mixes with sperm from your testicles to make semen. It also produces a protein called prostate-specific antigen or PSA. PSA helps reduce the thickness of semen, so it becomes more liquid.
If you have been diagnosed with prostate cancer, it means there is a lump of tissue inside your prostate (a tumour) that has cancer cells inside it that will divide and grow. Once the tumour breaks through the prostate wall, the cancer cells can spread to other parts of your body. Find out more about prostate cancer, tests, and treatments.
What causes prostate cancer?
The exact cause of prostate cancer is unknown. But certain things increase a man’s chance of developing it. These are called risk factors. Having a risk factor for cancer does not mean a man will get prostate cancer; it just means he has an increased risk.
About hormone therapy
What is hormone therapy?
Testosterone (the male sex hormone) causes prostate cancer to grow. The most common way of controlling how much testosterone there is in your body is to have hormone therapy (also known as androgen deprivation therapy or ADT). Your doctor may recommend hormone therapy to reduce the amount of testosterone in your body. Treatments include injections, implants, tablets, or a nasal spray.
The type of treatment you are offered will depend on the stage and grade of your cancer, but the most common categories of treatment are shown below:
About cardiovascular disease
What is cardiovascular disease?
Cardiovascular disease is a term used to describe conditions that affect the heart or blood vessels. Fatty deposits can build up inside the blood vessels causing blockages. These blockages are extremely dangerous. They can restrict the blood supply to the heart or brain, leading to fatal heart attacks or strokes.
Cardiovascular disease is common in men with prostate cancer. So, you need to remain healthy and look after yourself, despite the physical and mental fatigue you may be feeling since your diagnosis or during treatment.
Am I at risk of cardiovascular disease?
Your risk of cardiovascular disease increases if you smoke, are overweight, do not exercise, suffer from high blood pressure (called hypertension), or have diabetes. If you have a family history of cardiovascular disease, then this may also increase your risk.
What is metabolic syndrome?
Metabolic syndrome is a combination of diabetes, obesity, and high blood pressure. It is a serious health concern.
If you have 3 or more of the following risk factors, you may have metabolic syndrome:
• increased blood sugar or an inability to control your blood sugar levels
• very overweight or have too much fat around your waist (94 cm or 37 inch waist in European men; 90 cm or 35 inch waist in South Asian men)
• high levels of fat (called triglyceride) and low levels of “good cholesterol” (called high-density lipoprotein) in the blood
• blood pressure readings consistently 140/90 mmHg or higher
• increased risk of developing blood clots (called thrombosis)
Having metabolic syndrome increases your risk of cardiovascular disease, which means you are at risk of having a heart attack, stroke, or other serious complication. You are at increased risk of developing metabolic syndrome if you are of African descent.
Link between hormone therapy and cardiovascular disease
What are the risks of having hormone therapy?
Hormone therapy is an effective treatment for men with prostate cancer, but nearly every treatment has risks or side effects.
Why does hormone therapy increase the risk of cardiovascular disease?
Hormone therapy causes changes in your metabolism and can affect your blood sugar levels, cholesterol, and how your body stores fat. These metabolic changes are known to lead to cardiovascular disease. More studies are needed to fully understand the link between hormone therapy and cardiovascular disease.
If you have the risk factors for cardiovascular disease, starting hormone therapy may increase your risk of developing cardiovascular problems during and after treatment. Therefore, your doctor should check it is safe for you to have your planned hormone therapy before you start treatment.
Watch our animated video about the risk of hormone therapy in patients who have cardiovascular disease.
Watch our video in which three experts from different disciplines explain cardiovascular considerations in prostate cancer patients on ADT.
What is a cardiovascular risk factor assessment?
If you have any of the following risk factors for cardiovascular disease, ask your doctor about a “cardiovascular risk factor assessment” before you start hormone therapy:
• Metabolic syndrome
• Heart problems, such as angina, heart failure, or a previous heart attack
• Blood vessel problems, such as carotid artery disease or peripheral artery disease
If you have already started hormone therapy treatment and think you have an increased risk of cardiovascular problems, talk to your doctor about having this done. If you are not sure if your doctor did a risk factor assessment before you started hormone therapy, you can check with your doctor for reassurance.
How is my risk of cardiovascular disease calculated?
Your doctor will assess the extent of your current cardiovascular problems, as well as looking at your family history. Your risk of developing a serious cardiovascular problem resulting from starting your planned hormone therapy will need to be determined. Your doctor may also use a risk assessment calculator to predict your risk of cardiovascular problems. These are statistical programmes that should only be used by healthcare professionals and not by patients themselves.
Your cardiovascular risk factor assessment results and predicted risk calculations will help your doctor decide which hormone therapy is the most appropriate for you. There are several types of hormone therapy, so some treatments may be better suited for you than others. If your risk of cardiovascular problems is high, your doctor may recommend medication or lifestyle changes to help reduce your risk of problems during your hormone treatment.
Reducing the risk of cardiovascular disease
How can I reduce the risk of cardiovascular disease?
Depending on the extent of your cardiovascular problems and calculated risk of future serious complications, your doctor may advise one or several ways of reducing your risk of developing cardiovascular disease. This may include medication, lifestyle changes, or surgery.
Medication
Your doctor may prescribe you medication to:
• Prevent your blood from clotting (called anti-platelets)
• Reduce your blood pressure (called anti-hypertensives)
• Reduce the amount of fat and cholesterol in your blood (called lipid-lowering drugs)
Lifestyle changes
Reducing your risk of cardiovascular disease requires changes to your lifestyle. This includes a healthy diet, keeping active, cutting down on alcohol, avoiding smoking, and looking after any other health problems you may have.
You may find it helpful to join an educational programme, such as Life on ADT or Feel+®. Life on ADT was founded by a research scientist who has been receiving hormone therapy for over a decade. Richard Wassersug wanted to help men and their families know what to expect when starting hormone therapy. The programme and accompanying book discuss ways of managing side effects, staying healthy, and maintaining your quality of life. The Feel+® programme has been designed to help you take control of your life and provide guidance on how to become more physically active. It provides tips on improving your food choices, and how talking about cancer can help you and your loved ones cope.
Some men can make simple lifestyle changes easily. But for others, as much as you may want to make those “simple” changes, it just seems too difficult. A pros and cons list may help you to persuade yourself just how important these lifestyle changes are. Or maybe talking to your family and friends and making the changes together will provide the supportive environment you need.
We have listed some tips and tricks below that you might find helpful.
Healthy diet
Changing your diet is not always easy. With so many ready meals available in the supermarkets, and the ease of ordering takeaways, it can be difficult to think about making meals from scratch. But you can help your body by eating as healthily and as sensibly as you can.
Your first step is to eat fewer foods high in calories, fat, salt, and sugars and swap them for something healthier, including more fruit and vegetables. Having high-quality, easy-to-prepare items in your food cupboard and refrigerator will help you stick to a healthy eating plan.
Below we have listed examples of healthy food alternatives:
| Breakfast | |||
| Swap this | For that | ||
| Sugar-coated cereal | ———————–> | Porridge with mashed banana | |
| Lunch | |||
| Swap this | For that | ||
| Tuna melt panini | ———————–> | Tuna salad on wholemeal bread | |
| Dinner | |||
| Swap this | For that | ||
| Beef burger and fries | ———————–> | Homemade turkey burger with sweet potato wedges | |
| Snacks | |||
| Swap this | For that | ||
| Full-fat yoghurt | ———————–> | Low-fat yoghurt | |
| Crisps | ———————–> | Rice crackers |
Keeping active
It is common for men undergoing hormone therapy to gain weight(as fat, typically around the belly and hips), and more so if you are not physically active. We know that exe rcise might be the last thing on your mind right now, but we encourage you to view exercise as an essential part of your overall treatment. It is also important to start exercising before noticing any weight changes; once you gain weight, it can be challenging to lose it.
Remember, whatever gets you moving counts as exercise! Going for a brisk walk, taking the dog for a run, going for a swim, doing the gardening, painting and decorating, housework, playing sports, or playing with the kids or grandkids, it all counts. So, if home exercises or the gym are not for you, try to plan more daily activities into your week to help keep you active.
If you are already physically active, we recommend you increase your activity to help maintain your weight.
Cutting down on alcohol
If you are in a routine of drinking alcohol, you could try these simple ideas to help you cut down:
- Using an alcohol measure when drinking spirits, or having a small (125 mL) glass for your wine, can help you cut down on your alcohol intake and calories.
- Try swapping strong beers or wines for lower strength alternatives. There is an increasing trend in no alcohol or low alcohol drinks in supermarkets, pubs, and other venues. Some of these alternatives are close in taste to the real thing! Did you know you can even buy no alcohol rum, bourbon, and gin?
- Let your friends and family know you are cutting down on alcohol so that they can support you. Feeling competitive? Why not set a challenge to see who can drink the least in a week!
Avoiding smoking
If you have been smoking for several years, are a social smoker, or reach for cigarettes in times of stress, we know that reducing or stopping smoking does not happen overnight for most people.
- Create a realistic plan to help you reach your goal and remind yourself why you are doing this.
- Let your friends and family know you are cutting down/trying to quit smoking so that they can support you.
- Talk to your doctor about nicotine replacement therapy.
Surgery
If your risk of cardiovascular disease is likely to be dangerously increased from starting hormone therapy, your doctor will want to discuss available options. In this situation, your doctor may talk to you about a surgical procedure called an orchidectomy. This operation involves the removal of the testicles. It is a straightforward operation that removes most of the flow of testosterone. It also means that some of the side effects of hormone therapy may not be an issue for you, but it is a procedure that cannot be reversed. You would need to be sure that this is the right treatment for you, given your risk of cardiovascular problems.
Living with cancer
What is it like living with prostate cancer and cardiovascular disease?
Being told you have cancer can be a big shock, even if you had prepared yourself for the possibility of your tests being positive. Although many people are cured of cancer or live with it for many years, a cancer diagnosis can cause different fears and emotions for you and your loved ones.
Combine this with hormone therapy, which will lower the amount of testosterone in your body, it is completely normal to be tearful or angry, or just not your usual self.
If we then throw being told you have an increased risk of cardiovascular disease or metabolic syndrome into the mix, it is easy to see how this can have a considerable impact on your mental health! We know being told you need to make lifestyle changes on top of everything else you are going through is the last thing you want to hear, but it really could extend or even save your life.
You may find it helpful to join a programme like Life on ADT or Feel+® to help you and your loved ones manage the side effects of treatment, improve your quality of life, and maintain strong intimate relationships while on hormone therapy.
It is important to know that you are not alone. If you are struggling, talk to your doctor about local support groups or counselling services that may be helpful to you and your loved ones.
How long will I need to have hormone therapy?
Some men need continuous hormone therapy; others take the treatment for a while and then stop and take a break, called intermittent therapy. Your doctor will discuss with you whether you need hormone therapy for life or intermittently. This largely depends on how well your cancer is controlled and how your PSA level behaves over time.
Intermittent hormone therapy can potentially limit the side effects of treatment while still maintaining good overall cancer control. However, intermittent hormone treatment requires regular monitoring of your PSA levels. Your doctor will agree a PSA level with you that, once reached, means you will need to start hormone therapy again. The periods off treatment may also get briefer as the years go by.