Table of Contents [hide]
Your doctor may suggest treatment to improve your nocturia. This section describes different treatments. Together with your doctor you can decide which approach is best for you.
Factors which influence this decision include:
- Your medical history
- Any other medication you are taking
- Drugs available in your country
- Your personal preferences and values
This section offers general information about treatment and situations can vary in different countries.
Watchful waiting
If your symptoms are only bothering you a little, watchful waiting can be an option. This means that you see your doctor regularly (usually every year) or when the symptoms become worse.
Over-the-counter supplements
You may want to try supplements which have not been prescribed by your doctor because you consider them more natural and safer. However, it is not entirely clear how these supplements work to relieve nocturia. It is also not clear how effective they are because their quality can vary greatly. Doctors do not recommend taking them to improve nocturia. If you take any supplements to relieve your symptoms, inform your doctor during consultation.
Muscarinic receptor antagonists
Muscarinic receptor antagonists (MRAs) are drugs which reduce the abnormal contractions of the bladder. They may reduce the sudden need to urinate which is difficult to postpone. There are several types of MRAs:
- Darifenacin
- Fesoterodine
- Oxybutynin
- Propiverine
- Solifenacin
- Tolterodine
- Trospium chloride
Mirabegron is a beta-3 receptor agonist. This medicine relaxes the bladder muscle and helps to increase the capacity of the bladder resulting in less need to urinate.
Side effects of MRAs are usually mild. They may include dry mouth and eyes, acid reflux, and constipation. In rare cases, they may cause symptoms of the common cold, blurred vision, and dizziness as well as difficulty urinating.
In the elderly, long-time use of MRAs may worsen the side effects. You should always follow your doctor’s advice about the duration of treatment.
Loop diuretics
In some patients, nocturia may be caused by improved blood circulation. When you lie down, it is easier for the heart to pump blood around the body, including your kidneys. Your body then produces more urine because the kidneys filter more blood, causing nocturia. To treat this, you can take a mild loop diuretic drug. Taking diuretics in the afternoon will drain excess fluid from your body during the day, rather than at night.
There are several loop diuretics available:
- Furosemide
- Bumetanide
- Torsemide
Side effects include dehydration, gout, low salt or low potassium levels in your blood, dizziness and low blood pressure.
Desmopressin
If your nocturia is caused by a decrease in the production of the hormone vasopressin (see What causes nocturia?), it can be replaced by the drug desmopressin. This drug helps reduce urine production by concentrating the urine and is recommended if you have nocturnal polyuria.
Desmopressin may reduce the number of times you wake up to use the toilet and allow you more hours of uninterrupted sleep. It comes as a tablet, a nasal spray, or a melt-in-the-mouth tablet and is taken right before sleeping. It is effective for 8-12 hours. The drug is available in various doses and women often need a lower dose than men.
Desmopressin can cause a drop in blood sodium levels. That is why it is common to have your blood tested before and during your treatment. Less common side effects are a headache, nausea, diarrhoea, pain in the abdomen, dizziness, facial flushing or dry mouth. In rare cases, desmopressin can cause high blood pressure and swelling of the feet and ankles (known as peripheral oedema).
Prostate medication and surgery
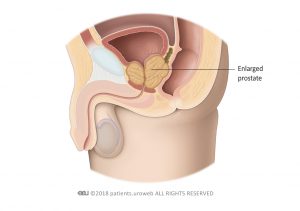
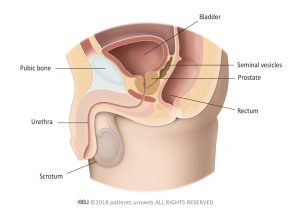
Because of the relationship between the prostate and the bladder, some men are prescribed medication to relax the muscle within the prostate gland or reduce the size of the prostate. This may improve their lower urinary tract symptoms (LUTS) but is less effective in improving nocturia.
In some cases, transurethral resection of the prostate (TURP) is recommended to improve the symptoms of benign prostatic enlargement (BPE) when it affects bladder function (Fig. 1 and 2). The surgery unblocks the bladder outlet by cutting away parts of the prostate. However, unless you have urinary symptoms during the day was well, TURP is unlikely to improve nocturia.