Table of Contents
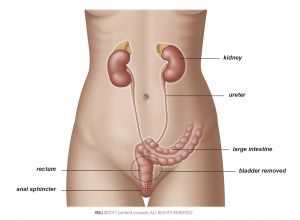
After removal of your bladder (cystectomy), you’ll need a new way to store and pass urine without a bladder. To do this, your surgeon will create a urinary diversion.
The three most commonly used urinary diversions are discussed:
- The ileal conduit (with urostoma)
- The neobladder (with internal urine pouch)
- Rerouting ureters through the skin (ureterocutaneostomy)
Other options may be available at your treatment centre. Your doctor will recommend the best type of urinary diversion for you based on your situation.
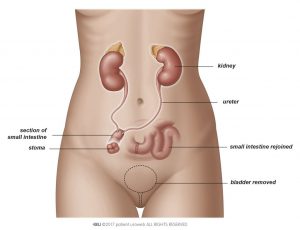
Ileal conduit
The ileal conduit is a new tube to carry urine out of the body. It is made from a section of your small intestine. The conduit runs from the kidney to an opening in your belly, called a stoma or a urostoma. Urine flows continuously through the opening and collects in a small bag placed over the stoma.
Your doctor or stoma nurse will give you instructions on how to change the bag when it becomes full. The bag fits under your clothes.
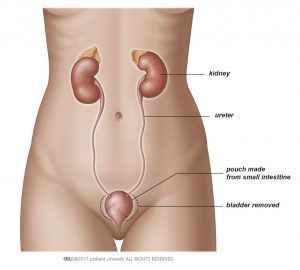
Neobladder
A neobladder is a pouch created from a section of your intestines to store urine inside your body. The neobladder is positioned in the same place as your original bladder. Ureters from the kidney connect to one end, and the urethra connects to the other end, just like in your original bladder. You will pass urine through the urethra.
If you have a neobladder placed, the tissue will need time to heal. A catheter will drain urine from the new bladder for a few weeks after surgery. Once the catheter is removed, you will need to wear pads while you relearn how to control your urine. Your nurse will teach you how to empty the neobladder. You will also learn pelvic floor exercises to strengthen your bladder control
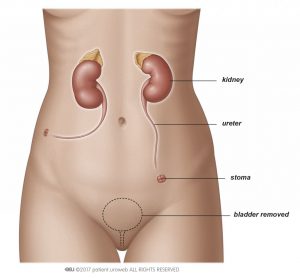
Ureterocutaneostomy
Rerouting ureters through the skin
By moving the ureters either together or individually to empty through a new opening in the skin (stoma) at the side of abdomen (Fig. 3), urine can simply exit the body into a stoma bag. This diversion is the most simple. Although it is rarely used, it is safe and feasible for patients who have medically complicated situations (prior operations, multiple health problems, palliative care) or who cannot care for themselves after the operation.
Other urinary diversions
Less commonly used urinary diversions are:
- Cutaneous urinary diversion
- Ureterocolonic diversion
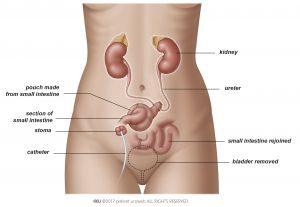
Creating a pouch or reservoir inside the body (cutaneous urinary diversion)
By using small intestine or large intestine and sometimes the appendix, a reservoir is created in the abdominal cavity and then connected to the skin with a valve mechanism. With this low-pressure pouch, urine can be stored within the body. The goal of this procedure is to allow control of emptying (continence) or backflow to the kidneys (reflux). The reservoir is emptied by intermittent catheterisation with a small plastic catheter every 2–6 hours. The opening can be anywhere on the lower abdomen or in the belly button (umbilicus).
If you choose this diversion, your eye–hand coordination must be sufficient to catheterise and drain the pouch regularly by yourself. Liver and kidney function must be adequate because of reabsorption of urinary components (salts, uric acid, water) by the intestinal lining of the pouch causes extra stress on these organs.
Complications include infections, incontinence, hernia, reflux, tightening of the opening (stenosis), and leakage as well as short bowel syndrome and metabolic and electrolyte imbalances.
Since this procedure is technically challenging, especially creating the valve mechanism is not always successful, this technique is not often used.
Implanting the ureters into the rectum (ureterocolonic diversion)
When the ureters are implanted in the rectum, the urine is stored in the rectal pouch (Fig. 5). The anus and pelvic floor control the passing of urine and must function properly. This diversion leads to faecal matter mixing with the urine, so urination and defecation happen simultaneously.
This technique has a high rate of infections, so it is used infrequently and only under certain circumstances. Short-term complications include recurring infections (including inflammation of the abdominal wall and the kidneys), tightening of the opening to the rectum, and leakage. Long-term complications include incontinence from having to void urgently, bowel irritation, and associated colon cancer.
Impact on life
Sex life after radical cystectomy
Ask your doctor or stoma nurse/specialised nurse when it’s safe to resume sexual activities. You should wait at least six weeks before sexual intercourse to allow proper healing to take place.
Your sex life might be affected after having surgery for bladder cancer. This depends on the type of surgery you have.
Your body may look different after the surgery, which may take time to get used to. For men, the penis may appear slightly shorter than before the surgery. For both men and women, having a stoma can also affect the way you feel about yourself and how you feel about having sex. Take your time to recover. You will feel when you are ready to start sexual intercourse again. In the meanwhile spend time with your partner, share interest, enjoy cuddling and do not stop talking with each other.
Men
Bladder removal for men typically includes removing the prostate. This is done to prevent bladder cancer coming back in the prostate later.
Without a prostate, you will not be able to produce semen fluid. You can still have an orgasm, but your orgasms will be dry (without semen). Sperm cells can still be produced in the testicles but you cannot make a partner pregnant by sexual intercourse. Talk with your doctor before surgery if you have questions about fertility.
Your ability to have an erection may be affected. Cystectomy can damage the nerves that control erection. Talk with your doctor if you have questions about sex or fertility.
If the nerves are not damaged, you might still need assistance to get an erection after surgery. Ask your doctor or nurse what techniques might work for you. Several options exist and can be used alone or together:
Medications to cause erection
- External devices like a vacuum pump, which draws blood into the penis to stiffen it
- Internal devices like pellets or a penile prosthesis that is implanted in the penis
Women
Bladder removal for women typically includes removing the internal sexual organs, including the uterus, ovaries and the part of the vagina that is next to the bladder and urethra. This is not necessary in every case, but is typically done to make sure all the cancer is removed. The labia and clitoris are not removed, and most of the vagina will usually be left, so most women will still be able to have an orgasm and intercourse.
It may take time to get used to how this looks and feels. Sex may feel different than it did before surgery. You might have less sexual desire. You might need to use a gel to help with lubrication. Treatment is available if intercourse is painful (dyspareunia). Talk with your partner and your doctor or nurse about these problems.