Table of Contents
What is TUMT?
Transurethral microwave therapy (TUMT) of the prostate is minimally invasive treatment which uses microwave energy to harden parts of the prostate tissue. This process is called coagulation. The treated part of the prostate is either absorbed by the body or it passes with urine after the procedure. The aim of TUMT is to reduce the prostate volume and to improve the symptoms.
When should I consider having TUMT?
TUMT is recommended for men with a prostate between 30 to 100 millilitres who prefer minimally invasive treatment or do not wish to have surgery because of other medical conditions
The procedure
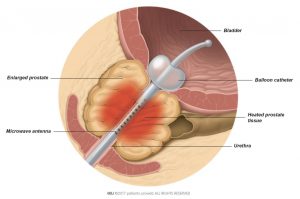
For Transurethral Microwave Therapy (TUMT) you will receive local anaesthesia which is sometimes combined with intravenous anaesthesia. Once you are under anaesthesia, the doctor enters the urethra with a catheter which has a microwave antenna and a balloon. The antenna heats up the prostate tissue with microwave energy and the balloon keeps the antenna in place inside the prostate (Fig. 1). After the procedure a different catheter will be placed in your bladder to help you urinate.
You will need this catheter for some days until the urethra is healed and you can urinate on your own. The catheter is removed by the urologist at the hospital or clinic.
How to prepare for the procedure
Your doctor will advise you in detail about how to get ready for the procedure. To prepare for the anaesthesia you should not eat, drink, or smoke for 6 hours before the procedure. If you are taking any prescribed medication, discuss it with your doctor. You may need to stop taking it before TUMT.
Treatment for urinary incontinence depends on the type of incontinence, how severe it is, and what may cause it. Often, self-management measures are combined with drug treatment. Together with your doctor you can decide which drug treatment is best for your situation.
The main types of medications used to manage incontinence are muscarinic receptor antagonists (MRAs), mirabegron, and oestrogen. Other drugs include desmopressin and duloxetine.
After the procedure
How long will it take me to get back to my daily activities?
In most cases, you can leave the hospital a few hours after TUMT. Do not drive a car when leaving the hospital because you may still be drowsy after the anaesthesia. Make sure you get enough rest on the day of the procedure.
With the catheter still in your urethra, you can start getting back to your daily activities the next day. Your urine may contain traces of blood which can last up to several weeks.
For 4-6 weeks after the surgery:
- Drink 1-2 litres every day, especially water
- Do not lift anything heavier than 5 kilograms
- Do not do any heavy exercise and avoid bike riding
- Do not take thermal baths or go to the sauna
- Prevent constipation by adapting your diet
- Discuss any prescribed medication with your doctor
Avoid having sex for 2-3 weeks. After TUMT, you may suffer from retrograde ejaculation. This is a chronic condition where semen can no longer leave through the urethra during orgasm. Instead it goes into the bladder and later leaves your body during urination. Your semen may be stained with blood for a few weeks.
You need to go to your doctor or back to the hospital right away if you:
- Develop a fever
- Face problems with the catheter
- Are unable to urinate on your own after catheter removal