Table of Contents
Types of tumours
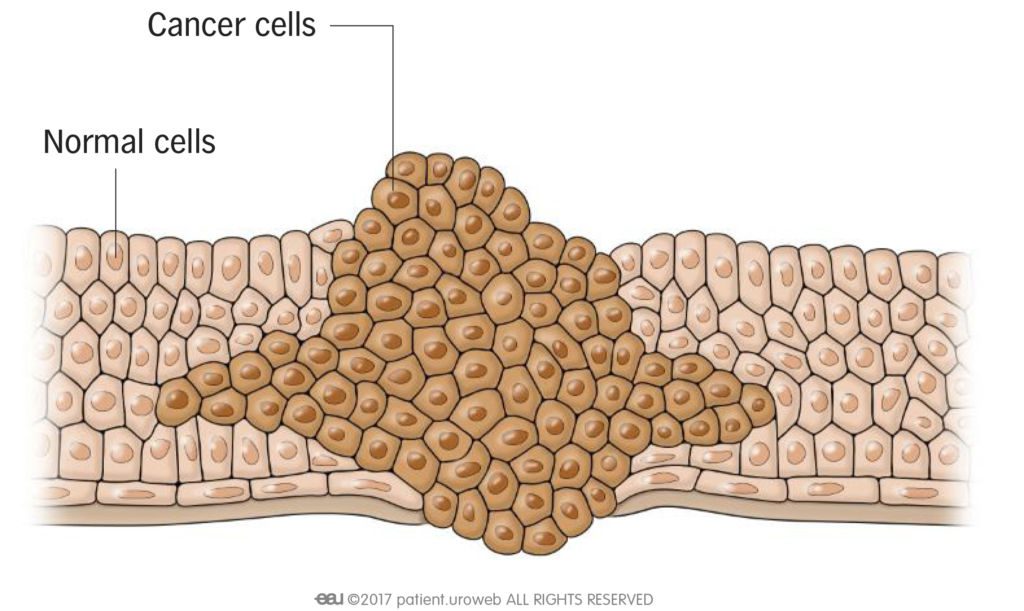
- Benign tumours are not cancer. They usually grow slowly and push away healthy tissue. They do not
spread to other parts of the body. If a benign tumour is large, it can press on other body organs or structures and cause bleeding or pain. - Malignant tumours are cancer. A malignant tumour is able to invade and destroy surrounding tissue.
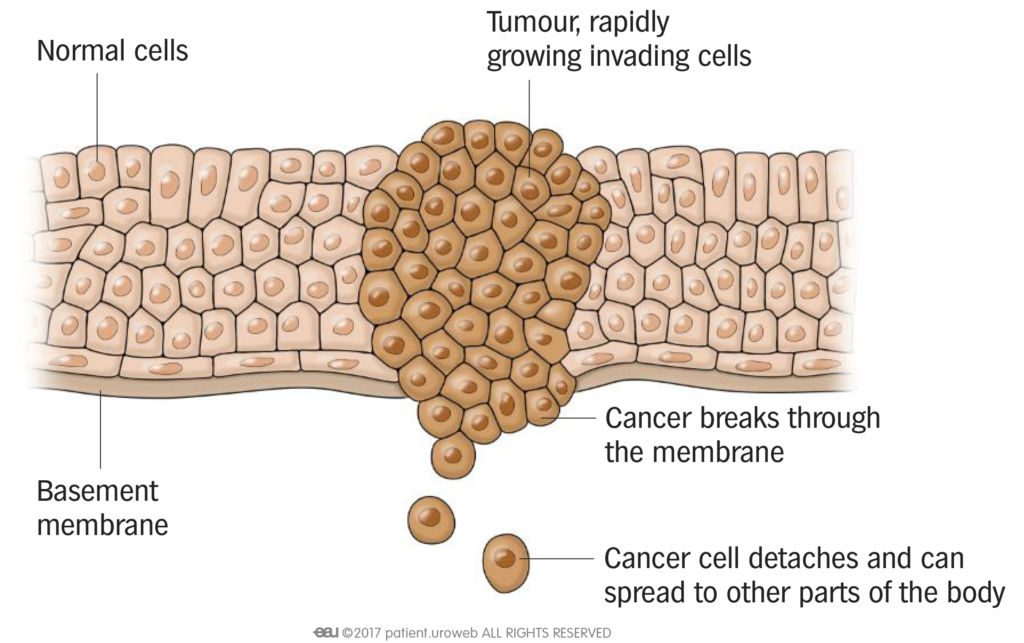
- Metastatic tumours grow from cancer cells that have travelled to another part of the body (Fig. 2).
The original tumour, called the primary tumour, is the source of the cancer cells. The new tumour is called the secondary tumour. Cancer cells can spread through the blood (haematogenous metastasis) or through the lymph vessels to the lymph nodes (lymph node metastasis).
Metastasis in prostate cancer
Prostate cancer can sometimes spread to the bones and cause another tumour to grow there. When this happens, the cancer cells from the prostate (primary cancer) have travelled with the blood to the bones. The new tumour (secondary cancer) is called a bone metastasis of prostate cancer.
Different cancers spread to common sites or organs, usually in a typical pattern. Cancer can spread to any part of the body, but this is more rare. The process of metastasis is complex, and many factors come into play. Of a few thousand cancer cells, it is thought that only few survive and are able to grow in another part of the body.
If the doctor thinks micrometastases are likely, drug therapy can be given to try to kill the remaining cancer cells before they can grow into macrometastases.
What causes cancer?
Cancer starts in the body’s cells. An unrepairable change or error of the genetic code of a cell may lead to mutation and cancer.
Not every mutation leads to cancer. Mutations can be inherited, which means they are in the genes already at birth, or they can occur during your lifetime. Mutations can occur by chance, without a known cause. Sometimes they are the result of stress caused by harmful substances in the environment, such as sunlight, air pollution, cigarette smoke, alcohol, or chemicals. Exposure to harmful substances can increase the risk of getting cancer.
Why does cancer sometimes come back?
Doctors do their best to destroy all cancer cells, but sometimes cancer comes back even after a long time. Cancer cells may have spread or gone into a state of rest somewhere in the body and eventually grow there. Sometimes not all cancer cells are removed during surgery or killed by chemotherapy or radiation; these cells can grow and produce a new tumour of the original cancer at the same place (relapse). In addition, cancer cells are very effective at adapting to new conditions and can become resistant to certain types of treatment.
After cancer treatment, you are scheduled for follow-up visits with your doctor. It is important to attend these visits. Your doctor can suggest additional treatment if there are signs of tumour cells remaining in the body.
Types of cancer
Cancer can arise from cells in different tissues and organs in the body (Table 1). For example, a primary cancer that develops in the breast is called breast cancer. Cancer will have different names depending on the tissue of origin.
The main group of cancers |
|
Carcinoma |
This cancer begins in epithelial cells. These cells line the surface of the skin, inner organs, and glands. It is the most common type of cancer and usually grows as a tumour. There are different types of carcinomas. For example, adenocarcinomas originate from the glands, squamous cell carcinomas from the skin, and urothelial carcinomas from the lining of the urinary system. |
Melanoma |
This cancer begins in pigmented cells. Melanomas usually develop in the skin but also can begin in inner organs. |
Sarcoma |
This cancer begins in different types of tissues in the body, such as bone (osteosarcoma) or “soft tissues” such as muscles, nerves, vessels, cartilage, and connective or fat tissue (soft tissue sarcomas). |
Lymphoma |
This cancer begins in the white blood cells in the lymphatic system, for example, in a lymph node. |
Leukaemia |
This cancer begins in blood-forming tissue such as the bone marrow and causes the tissue to produce abnormal blood cells. This type of cancer usually does not form a solid tumour. |
Brain and spinal cord tumours |
These tumours arise from nerve cells in the brain and spinal cord, called the central nervous system, and usually are limited to this site. |
How is cancer diagnosed?
Your doctor might notice signs or symptoms of cancer during a medical examination. If cancer is suspected, some tests are performed. A physical examination is carried out and some form of imaging will take place. Small quantities (samples) of blood and/or tissue from your body are often taken to be studied by a pathologist. The pathologist uses a microscope and special techniques like cell staining and molecular tests to make the diagnosis.
Cancer classification
To understand and treat your cancer, the doctor needs to know:
- Has the tumour grown into the surrounding tissue?
- Are the lymph nodes involved?
- Have the cells spread to other organs?
Your doctor uses this information to classify the cancer with the tumour node metastasis (TNM) staging system.
What is the TNM staging system?
TNM stands for Tumour (T), lymph Node (N) and Metastasis. This classification is widespread and accepted internationally. It is used to determine the stage of a solid cancer and provides prognostic information. This means that the doctor can estimate the risk of disease progression and recurrence using the TNM-classification. Classification and staging are important for determining the best treatment.
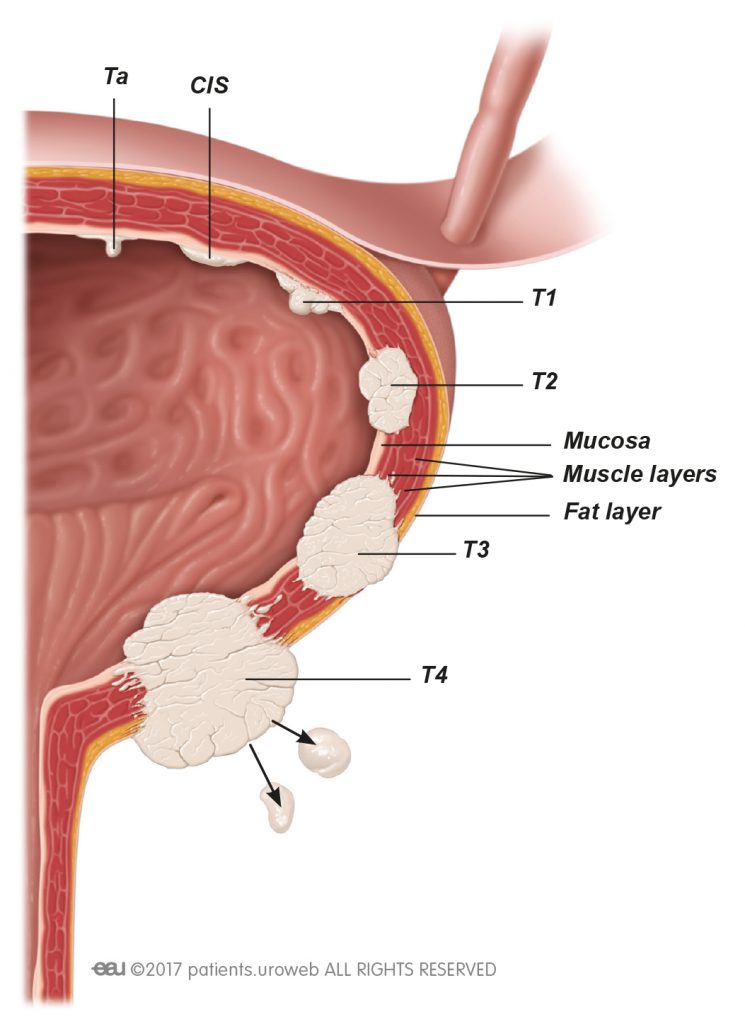
Tumour stage indicates the size of the tumour and/or whether the cells have invaded adjacent tissue (local invasion). Tumours are classified as T0 (no signs of a tumour), Ta (superficial swelling of normal tissue), Tis or Cis (superficial cancer, called carcinoma in situ) and T1 to T4 (extent of local invasion) (Fig. 3). Tx means that the tumour cannot be evaluated.
What is local invasion?
When cancer tumours spread to the healthy tissues immediately surrounding the tumour, we call it local invasion. Local invasion is therefore different from metastasis, which is cancer that has spread to distant locations in the body.
- Tumour grade provides additional information about how similar the cancer cells are to the cells of origin. Grading is indicated as G1, which means that a cancer is quite similar to the cells of origin, to G3, meaning the cells are not similar. A G4 cancer is undifferentiated, the most aggressive type. Tumour grade can be assessed only under a microscope, usually by a pathologist.
- Lymph node status indicates possible lymph node metastases. When a tumour is removed, often some of the lymph nodes in the tumour’s region are also removed. This is done to find and get rid of possible lymph node metastases. The number of lymph nodes removed is different in every case because all our bodies have different numbers and distributions of lymph nodes. The lymph node status is indicated as Nx when lymph node status cannot be determined, N0 when no lymph node metastases are present, and N1 to N3 depending on the number, size, and/or site of lymph node metastases.
- Metastasis status is also classified. M0 indicates that no metastasis is evident. M1 indicates that cancer cells have spread to other organs or tissues.
This information has strong relevance for treatment and possible outcomes (prognosis). Additional detail is available depending on the type of cancer and overall situation.
What is CUP syndrome?
CUP is an abbreviation for Cancer of Unknown Primary. It means that a cancer metastasis is detected somewhere in the body, but the origin is not known. Sometimes the primary cancer cannot be detected, even after extensive examinations. There are special therapies for this type of cancer.
How is cancer treated?
Treatment is based on your type of cancer as well as your overall health and preferences. It may involve surgery, chemo-/immunotherapy, or radiation, or combinations. Clinical trials may be available to study new treatments such as immunotherapy or gene therapy. Your doctor works with a multidisciplinary team to guide your treatment.
Cure or remission?
A lot of cancers can be cured today, but your doctor might hesitate to tell you that. Some cancer cells might have remained somewhere and are too few to cause symptoms, cannot be detected, or are dormant. This state is called remission, which means that no cancer is detectable at this time. When your cancer is in remission, only time can tell whether it is cured or not. You may still get check-ups, scans, or even get treatment to remove remaining cancer cells.
Interpreting cancer statistics – How to read the numbers
Statistics cannot tell what exactly will happen to you, but they provide good general indications. Because every cancer is unique, no statistic can give exact answers about the outcome of your cancer.
All statistical measures regarding Europe were taken from the EUCAN fact sheets http://eco.iarc.fr/eucan/CancerOne.aspx?Cancer=29&Gender=1
| Incidence | The number of people who had a new diagnosis of cancer during a certain period of time within a defined population. Example: The incidence rate of prostate cancer in Europe was 92 cases per 100 000 persons in 2012. |
| Prevalence | The number of people who had a certain type of cancer in a defined period of time. Example: In 2012, the average number of men with prostate cancer in Europe was 125 in 100 000 in a 1-year period and 490 in 100 000 in a 5-year period. |
| Mortality | The number of people with a certain type of cancer who died from the disease. Mortality data have to be read with care and with regard to incidence and prevalence. Example: Although in Europe 92 247 men died from prostate cancer in 2012, the 5-year prevalence was 1 459 627, making the number of deaths a small proportion (6.3%). It also means that the men who had prostate cancer had it for a long time and only few died of it. |
| Survival rates | The percentage of people who were alive with cancer after 1, 5, or 10 years. This information does not say anything about the individual course of cancer. |
| Overall survival | The survival rate in a defined population without taking the disease or cancer into account. For overall survival, it does not matter if a person died from cancer or for another reason, for example, a heart attack. |
| Disease-specific survival | The survival rate for the cancer. This rate does not take other causes of death into account. |
| Survival by stage | The survival rates for cancer stratified by stage. The stage used for stratification is the stage of cancer at the time of diagnosis. |
| Cancer risk | The likelihood of getting a certain cancer in a defined period of time or over a lifetime. Example: The lifetime risk of developing prostate cancer was 1 in 8 in the UK in 2012, which means that 1 man out of 8 will develop detected prostate cancer at some point of his life, which equals a 12.5% chance. This does not allow individual prediction of the risk of getting a certain cancer, which is based on different specific factors. It is a cumulative risk, which means that it increases as you get older. Consequently, the risk is lower for an average younger person. |