Table of Contents [hide]
- 1 What is bladder cancer?
- 2 The function of the bladder
- 3 Stages of the disease
- 4 Signs and symptoms of bladder cancer
- 5 Diagnosis of bladder cancer
- 6 Treatment of non-muscle invasive bladder cancer
- 7 Treatment of muscle-invasive bladder cancer
- 8 Treatment of metastatic bladder cancer
- 9 Treatment options for metastatic disease
- 10 Treatment of recurrent bladder cancer
- 11 General information about bladder cancer
What is bladder cancer?
Bladder cancer is the growth of abnormal tissue (tumour) in the bladder. There are several stages of bladder cancer. Your treatment and experience will depend on the specific characteristics of the tumour (referred to as “staging” the tumour) and the expertise of your medical team.
This section provides general information about bladder cancer, diagnosis, and various treatment options. Discuss with your doctor what is best in your individual situation.
Stages of the disease
A tumour that grows towards the centre cavity of the bladder without growing into the muscle tissue of the bladder is called non-muscle invasive. These tumours are superficial and represent an early stage. This is the most common type of bladder cancer. In most cases, these tumours are not aggressive and rarely spread to other organs, so they are not usually lethal, they can however appear again (=recurrence) or develop aggressive features (=progression).
As the cancer grows into the muscle of the bladder and spreads into the surrounding muscles, it becomes muscle- invasive bladder cancer. This type of cancer has a higher chance of spreading to other parts of the body (metastatic disease) and is harder to treat. In some cases, it may be fatal.
If bladder cancer spreads to other parts of the body such as the lymph nodes or other organs, it is called locally-advanced or metastatic bladder cancer. At this stage, cure is unlikely, and treatment is limited to controlling the spread of the disease and reducing the symptoms.
Signs and symptoms of bladder cancer
Blood in the urine is the most common symptom when a bladder tumour is present. Tumours in the bladder lining (non–muscle-invasive) can cause a burning sensation and discomfort when passing urine as well as a need to urinate more often.
If you have urinary tract symptoms such as painful urination or need to urinate more often, a malignant tumour might be suspected, particularly if an infection is ruled out or treated and this does not reduce the symptoms. Muscle-invasive bladder cancer can cause symptoms as it grows into the muscle of the bladder and spreads into the surrounding muscles.
Symptoms like pelvic pain, flank pain (flank pain is pain on your sides, just below your ribs and above your hips. It’s the area around your lower back, where your kidneys are located), weight loss, or the feeling of a mass in the lower abdomen may be present in some cases when tumours are more advanced.
Diagnosis of bladder cancer
Your doctor will take a detailed medical history and ask questions about your symptoms. You can help your doctor by preparing for the consultation:
- Make a list of your previous surgical procedures.
- Make a list of the medications that you take.
- Mention other diseases and allergies that you have.
- Describe your lifestyle, including exercise, smoking, alcohol, and diet.
- Describe your current symptoms.
- Note how long you have had the current symptoms.
- Family history of other tumours, especially in the urinary tract.
Markers for bladder cancer
Both patient and tumour characteristics guide treatment decisions and prognosis of patients. Early detection of bladder cancer can improve the chance of successful treatment. Therefore, doctors try to find urine biomarker tests, which will help to identify bladder cancer or recurrence of bladder cancer as early as possible.
Urinary cytology is a test that examines your urine or bladder fluid for cancer cells. It is very good at finding aggressive, high-grade cancers, but might miss less aggressive, low-grade ones.
Cystoscopy
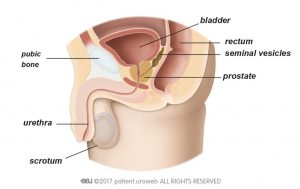
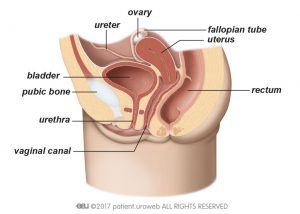
Cystoscopy is the main test used to diagnose bladder cancer. During this test, your doctor will insert a cystoscope, which is a thin tube with a camera and light on the end, through your urethra and into the bladder.
Newer, flexible cystoscopes are now available and easier to use, hence, patients are more likely to comply, especially men. Currently, urine tests cannot replace the need for a cystoscopy.
CT Urography
Computed tomography (CT scan) urography gives your doctor information about possible tumours in the kidneys or ureters and information about the lymph nodes and abdominal organs.
CT urography cannot detect small or superficial tumours (CIS). If small or superficial tumours are suspected further tests are needed.
Intravenous urography
Intravenous urography (IVU) is another imaging technique for examining the urinary tract. IVU may be used for the assessment of the upper urinary tract when CT-urography is not available. It cannot detect small or superficial tumours (CIS), and it’s not recommended for detecting lymph nodes or invasion of neighbouring organs.
Transabdominal ultrasound
Use of sound waves to create an image of the body’s inner workings. It cannot detect very small or superficial tumours (CIS). This study does not require intravenous contrast; however, ultrasound cannot replace CT urography or cystoscopy.
Transurethral resection of bladder tumour
Transurethral resection of bladder tumour (TURBT) is the surgical removal (resection) of bladder tumours. This procedure is both diagnostic and therapeutic. It is diagnostic because the surgeon removes the tumour and all additional tissue necessary for examination under a microscope (histological assessment). TURBT is also therapeutic because complete removal of all visible tumours is the treatment for this cancer. Complete and correct TURBT is essential for good prognosis. In some cases, a second TURBT is required after several weeks.
The decision to treat a bladder cancer further after TURBT is determined by the aggression of the cancer cells (the grade) and the extent of the cancer in the bladder (the stage as outlined above).
Photodynamic Diagnosis (Blue light cystoscopy)
In some cases, photodynamic diagnosis (PDD) is used during cystoscopy or TURBT to help the surgeon find tumour cells which could otherwise be missed. This technique involves introducing a dye (Hexvix®) into the bladder an hour before the surgery. The dye is absorbed by cancer cells which makes these cancer cells glow red under a blue light during surgery.
PDD can also be used during follow-up cystoscopy. Your surgeon will decide whether this is necessary for you.
Narrow-band imaging
Narrow-band imaging (NBI) is the application of light at specific blue and green wavelengths on the inner lining of the bladder during normal cystoscopy. This enhances the visual contrast between healthy tissue and cancer tissue and improves the detection of tumours in the bladder. This method does not require any bladder instillation.
Treatment of non-muscle invasive bladder cancer
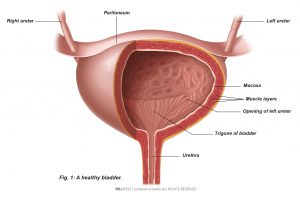
Non–muscle-invasive bladder cancer, also called superficial bladder cancer, is a superficial cancer that has not grown into deeper layers of the bladder wall (Fig. 3).
There are three subtypes based on how they grow:
- Stage Ta tumours are confined to the bladder lining.
- Stage T1 tumours have invaded the connective tissue under the bladder lining but have not grown into the muscle of the bladder wall.
- Stage Tis tumours are flat velvet-like tumours, also known as carcinoma in situ (CIS), that are confined to the bladder wall but have potentially a high risk of spreading into the deeper layers of the bladder.
Stage Ta and T1 tumours usually appear as small grapelike growths (also called papillary) that grow toward the centre of the bladder without growing into the deeper bladder layers. Your surgeon may remove these growths using a method called transurethral resection of bladder tumour (TURBT).
Transurethral resection of bladder tumour
TURBT is the surgical removal (resection) of bladder tumours. This procedure is both diagnostic and therapeutic. It is diagnostic because the surgeon removes the tumour and all additional tissue necessary for examination under a microscope (histological assessment). TURBT is also therapeutic because complete removal of all visible tumours is the treatment for this cancer. Complete and correct TURBT is essential for good prognosis. In some cases, a second surgery is required after several weeks.
Outpatient removal of tumour recurrence using laser
If a bladder tumour comes back (recurs) and was previously considered low-risk, it can often be removed using a laser.
In this procedure, a numbing solution is first injected into your bladder through a catheter. Once the numbness takes effect, the doctor uses a cystoscope and a laser beam to remove the tumour.
This procedure is usually done on an outpatient basis, meaning you can go home the same day. It’s similar to the cystoscopy you had when you were first diagnosed with the tumour.
Instillation treatment
As noted earlier, TURBT can eradicate stage Ta or T1 tumours, but some tumours commonly recur and can progress to invasive cancer. Intravesical (within the bladder) instillation treatment after TURBT should be considered for all patients.
Treatment of muscle-invasive bladder cancer
About a quarter of patients diagnosed with bladder cancer have a muscle-invasive form that has grown into the muscular part of the bladder wall (stages T2–T4). This type of cancer has a higher chance of spreading to other parts of the body (metastatic) and needs a different and more radical form of treatment. Muscle-invasive bladder cancer will be fatal if untreated.
Additional diagnostics
Computed tomography (CT scan) is particularly important for further work-up in muscle-invasive bladder cancer. With a CT scan of the thorax (chest area), abdomen and pelvis, done in less than 10 minutes, the physician can tell if the cancer has already grown out of the bladder and into the surrounding tissue or adjacent organs and if there are signs of spreading to other organs (metastatic disease). By adding intravenous contrast agent, which is excreted into the urine by the kidneys, the urinary tract above the bladder can be visualised and tumour growth identified.
Prior to treatment, it is essential to evaluate whether the cancer is metastatic. If the CT scan indicates that the cancer has spread to your soft (visceral) organs, your bones or lymph nodes, this will possibly change the treatment decisions.
Additional magnetic resonance imaging (MRI scans) or bone scans may be performed, although this is not routinely done. Bone and brain metastases are rare at the time that muscle-invasive bladder cancer is diagnosed. Therefore, your doctor would only consider a bone scan or additional brain imaging if you have specific symptoms that suggest bone or brain metastases. Unclear findings might also be probed with a needle biopsy to confirm metastatic disease.
A combination of positron emission tomography (PET scan; uses a radioactive tracer) and CT scan (PET/CT) is increasingly being used in European centres, although it is not generally available in all countries. PET/CT may improve the ability to detect distant metastases. It is not recommended for staging bladder tumours because urinary excretion of the radioactive tracer makes tumour staging very difficult.
Prognosis and risk stratification
The long-term prognosis for patients with muscle-invasive bladder cancer is determined by the extent of tumour growth (stage). As opposed to non-muscle-invasive bladder cancer aggressiveness (grade) which is determined by the pathologist is less important, since virtually all invasive tumours are high grade.
Removal of the urinary bladder (cystectomy)
The mainstay of treatment for muscle-invasive bladder cancer is surgical removal of the urinary bladder.
Bladder-sparing treatments
A bladder-sparing approach is currently used in a minority of cases worldwide but deserves consideration. Bladder preservation can be achieved at the cost of multiple therapies, including their side-effects. Transurethral resection of the bladder tumour (TURBT) and radiation is used to cure or control the tumour locally. Chemotherapy is used to treat the cancer cells that might already have spread within in the body (systemic disease). The goal is to preserve the bladder and its function as well as quality of life without compromising cancer treatment.
Studies in selected patient groups have shown good results for bladder-sparing approaches, about a third of patients still undergo bladder removal after failure of a bladder-sparing treatment.
Transurethral resection of bladder tumour
If you cannot undergo extended surgery, TURBT is possible if the tumour invades only the inner muscle layer of the bladder. With high recurrence and progression rates, this treatment alone cannot be considered a good option for controlling the disease long term.
Chemoradiation
Radiation therapy combined with sensitising chemotherapy is a reasonable alternative for patients who refuse or are not candidates for bladder removal. Evaluation of this approach will consider general fitness (life expectancy), kidney function, prior radiation, prior abdominal operations, and history of other cancers. A consultation with a radiation oncologist is advisable prior to deciding on this treatment.
Radiotherapy
Radiation therapy is an option for preserving the bladder in patients who are not candidates for surgery or who do not want surgery. Results from radiotherapy alone are worse than those from complete removal of the bladder, but if combined with chemotherapy (chemoradiation), acceptable results can be achieved. Side effects include mild to strong irritation of the bladder and digestive tract as well as incontinence, increased risk of infections, and fistulas (abnormal passages that develop between organs).
Chemotherapy
Chemotherapy alone has only limited results and is not recommended as a sole treatment.
Treatment of metastatic bladder cancer
Prognostic factors and treatment decisions
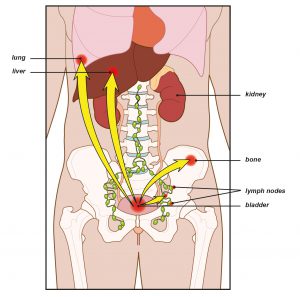
If your bladder cancer has spread to another body organ (Fig. 4), treatment is unlikely to cure you. Treatment options are limited to controlling the spread of disease (metastasis) and reducing symptoms. Certain drugs (Thiazolidinediones) should not be used for metabolic control in diabetic patients with bladder cancer.
Treatment options for metastatic disease
Chemotherapy
In 90-95% of bladder cancer cases the cancer type is urothelial carcinoma. Chemotherapy that contains platinum drugs used to be the main treatment for this type of cancer. But nowadays, a combination of treatments is preferred.
The first choice for treatment is a combination of two drugs: enfortumab vedotin (EV) and pembrolizumab. If EV isn’t suitable for you or isn’t available, your doctor might use cisplatin or gemcitabine along with nivolumab instead. If you can’t use these newer treatments, chemotherapy alone may be used.
Common side effects of these treatments include:
- Fatigue
- Tingling or numbness
- Loss of appetite
- Rash
- Hair loss
- Nausea
- Changes in taste
- Diarrhea
- Dry eyes
- Itching
- Dry skin
These side effects can vary, so be sure to discuss with your doctor if you are experiencing any of these side effects.
Chemotherapy combinations like gemcitabine and cisplatin are commonly used for bladder cancer. However, these treatments have side-effects that must be considered carefully if you cannot recover from your illness and the goal is to optimise your quality of life. Limited ability to perform daily activities (low performance status), other illnesses, or decreased kidney function could make you ineligible for these chemotherapies.
If your kidneys aren’t working well or you can’t take cisplatin, or if the combination of enfortumab vedotin (EV) with a checkpoint inhibitor (CPI) isn’t right for you, treatment with a CPI alone, such as pembrolizumab or atezolizumab, could be a good option.
Should your disease recur or progress while taking these therapies, your doctor may change your treatment to another type of therapy, depending on the treatment you’ve already received. Since there is no standard in this case, the choice will depend on your treating physician.
Additional surgery to remove a metastatic or recurrent tumour mass is used only to relieve pain or obstruction and will not cure the disease. Radiotherapy can also be used to treat symptoms like pain or recurrent bleeding (haematuria).
Some types of chemotherapy are quite intensive and can have a lot of side-effects. If you are not fit or if you feel unwell from the cancer, these side-effects can be quite severe. Older patients in particular may benefit from less intensive types of chemotherapy.
Immunotherapy
Patients that are unfit for regular Chemotherapy might be candidates for Immunotherapy (PD-L1) if genetic testing shows that they are sensitive to it.
Treatment of bone metastases
When bladder cancer has spread to the bone, skeletal complications can occur, such as weakening of the bones or pathological fractures from minor incidents or everyday activity. This causes pain and can have a detrimental effect on your quality of life. Your doctor may suggest radiotherapy, or drug treatment to help strengthen your bones and control the pain.
Access to clinical trials
All patients with a diagnosis of recurrent or metastatic bladder cancer, and particularly those whose prior chemotherapy has been unsuccessful, should be considered for centres where clinical trials are available.
A limited but increasing number of studies are available in various settings for patients who have never had chemotherapy as well as pre-treated patients. In addition, the recent experimental use of drugs called ‘immune checkpoint inhibitors’ in advanced bladder cancer appears effective in a subset of patients with this disease.
Deciding on treatment
If treatment is intended to slow down the cancer and control the symptoms, deciding what treatment is best for you—or whether to have treatment at all— can be very difficult.
You will need a clear understanding of what drug treatment can do for you at this stage and how it will affect your quality of life.
Talk to family or friends and people who are close to you. It can help to discuss things with someone outside your inner circle. Your doctor may be able to refer you to a counselor or specialist nurse.
Efforts are being made to promote patient advocacy for bladder cancer. Ask your oncologist if a bladder cancer patient representative is available near you.
Treatment of recurrent bladder cancer
Local recurrence of bladder cancer
Local recurrence takes place in the soft tissue where the bladder has been before removal or at the site of the lymph nodes that were removed. This is due to the fact that even after removal of the local pelvic lymph nodes, some nodes are left in place. Most local recurrences appear within the first 2 years. Local recurrence after complete removal of the urinary bladder is associated with poor overall prognosis but can occasionally be treated (surgery, chemotherapy, targeted radiation therapy).
Distant recurrence of bladder cancer
If the cancer recurs outside the pelvis, it is a distant recurrence. This type of recurrence is fairly common after bladder removal in patients with high risk of recurrence (larger tumours, positive resection margins, involvement of the removed lymph nodes). Distant recurrence happens mostly within the first 2 years after bladder removal. Sites of distant recurrences are lymph nodes, lungs, liver, and bones. Distant recurrence can be treated only by chemotherapy. Single or very few metastases may be surgically removed in addition to systemic treatment (= chemotherapy).
Medical trials might be available for your situation. Ask your doctor about these options.
Recurrence in the urothelial tract (urethra and ureters)
After complete removal of the bladder, the cancer can recur in the urethra, ureters and pyelum (urothelial tract).
Most recurrences of the urothelial tract happen within the first 3 years after the operation. This type of recurrence is relatively rare.
If possible, a local treatment such as surgery should be chosen to eliminate the cancer, unless it is suspected that the cancer has spread to other organs in the body (metastatic disease) In that case, chemotherapy is a treatment option, but the side-effects must be considered carefully if you cannot recover from your illness and the goal is to optimise your quality of life. In local treatment, the use of adjuvant radio therapy in addition to chemotherapy may reduce the chance of the cancer coming back.
In case of bladder preserving therapy and a superficial (non–muscle-invasive) recurrence, washing the bladder with drugs to prevent the growth or spread of cancer cells (instillation therapy) is advised.
Risk factors for recurrence in the urethra after removal of the bladder:
- Prior superficial (non–muscle-invasive) bladder cancer
- Multiple bladder tumours
- Tumour involvement of the bladder neck (and/or the prostate in men)
- An unused/residual urethra after incontinent urinary diversion
- Local recurrence in the lower pelvis
Although routine removal of the urethra (urethrectomy) is considered overtreatment, monitoring of the urethra is indicated in men.
Risk factors for recurrence in the ureters after removal of the bladder:
- Prior superficial (non–muscle-invasive) bladder cancer
- Multiple bladder tumours
- Tumour involvement at the opening (orifice) of the ureter
- Local recurrence in the pelvis
For patients with risk factors for urothelial recurrences, stringent or adapted monitoring is indicated.
General information about bladder cancer
Causes and risk factors for bladder cancer
What causes bladder cancer?
Several biological factors and harmful substances can increase the risk of developing bladder cancer. A higher risk does not necessarily mean that someone gets cancer. Sometimes bladder cancer develops without any known cause.
Risk factors for bladder cancer
Bladder cancer develops slowly and is more common in older people (age 60 and older). According to the European Association of Urology’s bladder cancer guidelines, tobacco smoking contains many harmful substances and is responsible for almost half of the bladder cancer cases.
Another well-known source of risk is occupational exposure to chemicals used in the production of paint, dye, metal and petroleum, although workplace safety guidelines have helped reduce this risk.
Infections from certain parasites and chronic urinary tract infections increase the risk of developing bladder cancer.
Classification and stages
Classification
Bladder tumours are classified by tumour stage and subtype and by grade of aggressiveness of the tumour cells. Staging is a standard way to describe the extent of cancer spread. The kind of treatment you receive will depend on these elements.
Stage and subtype
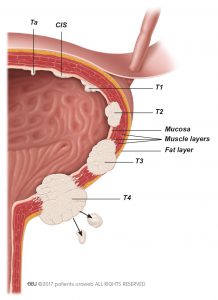
Tumour stage is based on whether or not the cancer has invaded the bladder wall (Fig. 3). This information is important for determining additional treatment and risk profile (the risk of recurrence of the disease).
Stages Ta, T1, and CIS indicate non-muscle invasive bladder cancer (Fig. 3):
- Ta tumours are confined to the bladder lining (shown as ‘mucosa’).
- T1 tumours have invaded the connective tissue under the bladder lining but have not grown into the muscle of the bladder wall.
- CIS tumours are flat velvet-like tumours that are confined to the bladder lining (shown as ‘mucosa’).
Stages T2, T3, and T4 indicate muscle-invasive bladder cancer, with tumours that have grown beyond the mucosa into the bladder wall (Fig. 3). Additional imaging of the abdomen and thorax (chest area) is used to detect tumour spread outside the bladder for staging of this type of bladder cancer.
Imaging for staging invasive bladder cancer
CT and magnetic resonance imaging (MRI scan) are the techniques used for staging invasive bladder cancer. A combination of positron emission tomography (PET scan; uses a radioactive tracer) and CT is increasingly being used in many centres in Europe to enhance the ability of detecting the spread of bladder cancer to the lymph nodes or other organs.
Imaging is used for staging invasive bladder cancer to determine prognosis and to provide information for treatment selection. Tumour staging must be accurate to ensure the correct choice of treatment.
In staging of muscle-invasive bladder cancer, imaging determines:
- How far the tumour has grown into the bladder wall (extent of local tumour invasion)
- Whether cancer has spread to the lymph nodes
- Whether cancer has spread to the upper urinary tract or other distant organs
Grading
During examination of tissue under a microscope (histological analysis), the pathologist will grade the tumours according to their potential to grow (aggressiveness). High-grade tumours are more aggressive, and tissue is greatly altered in appearance. Low-grade tumours are less aggressive, and tissue is mildly altered in appearance.
Stratification into risk groups of non-muscle invasive bladder tumours
For non-muscle invasive bladder tumours, risk stratification is used to provide more precise treatment recommendations. Your doctor does this based on disease stage and grade and some other tumour-related factors, and study-based risk tables.
You will be assigned to one of three groups (low, intermediate, or high risk) based on your risk of recurrence and progression. This stratification is used to determine the treatment options that can be offered and the follow-up that will be needed.
- Low risk: Patients have a single small (<3 cm) tumour that is stage Ta and that is not likely to grow (low grade). Low-risk patients do not have CIS, which has a high risk of growing into the deeper layers of the bladder muscle tissue and spreading to other organs or lymph nodes.
- Intermediate risk: Patients with tumours that are not clearly either low or high risk are considered to have an intermediate risk of recurrence and progression.
- High risk: Patients are at high risk if their tumour is stage CIS or T1 or is aggressive (high grade). Multiple large (>3 cm) and recurrent tumours of stage Ta are also high risk.
Bladder cancer prevention
A higher risk does not necessarily mean that someone gets cancer. Sometimes bladder cancer develops without any known cause.
It is important to maintain a healthy lifestyle. If you smoke, try to stop. Follow workplace safety rules and avoid exposure to harmful chemicals. Some evidence suggests that drinking a lot of fluids, mainly water, might lower bladder cancer risk. Eating a balanced diet with lots of fruits and vegetables has health benefits and might protect against cancer. If you have questions or need support to maintain a healthy lifestyle, ask your healthcare team for assistance or referrals.
Follow-up bladder cancer
After any kind of cancer treatment follow-up is essential to minimise complications and to detect and treat recurrences early. After complete removal of the bladder or other treatments, you will be asked to see your general practitioner, urologist, oncologist, radiologist, or a nurse practitioner at specific, fixed time intervals for monitoring and evaluation.
Your doctor may prescribe a drug known as pharmacological thrombo-prophylaxis for a period of 4 weeks to reduce the risk of blood clots.
A specialist should have the lead in coordinating and interpreting all of the results from the follow-up visits. That specialist—in most countries, the urologist— should also be the main contact for questions about your disease or related issues.
Symptoms of complications
After monitoring of cancer, the functional results must be observed and controlled. Functional complications after bladder removal include:
- Vitamin B12 deficiency
- High acid levels in the blood (metabolic acidosis)
- Worsening kidney function
- Urinary infections
- Urinary stone formation
- Tightening of stoma openings (stricture)
- Other stoma complications in patients with ileal conduit diversions (leakage, inversion, skin irritation)
- Neobladder continence problems, and emptying dysfunction.
Ask your doctor for information about the major symptoms of these complications and their prevention.
Learn more and find support at World Bladder Cancer Patient Coalition (WBCPC).